by Justin Mckibben | Jun 5, 2018 | Addiction, Anxiety Disorder, Depression, Dual Diagnosis, Mental Health, Mood Disorders, Post-traumatic Stress Disorder, Recovery, Veterans, Violence

(This content is being used for illustrative purposes only; any person depicted in the content is a model)
In 2010, the United States Congress declared June 27th as PTSD Awareness Day. In 2014, the Senate designated the entire month of June as National PTSD Awareness Month. The purpose of this observation is to raise public awareness of PTSD and promote effective treatments to help those who suffer.
So what is PTSD? And how can all of us help?
Understanding PTSD
PTSD stands for Post-Traumatic Stress Disorder, which is a mental disorder that can develop when someone is exposed to a traumatic event. Some of the most common experiences that cause PTSD include:
- Warfare
- Sexual Assault
- Traffic collisions
- Life-threaten events
Sometimes people can experience post-traumtic stress disorder even if they are not directly affected by the event directly. According to the American Psychiatric Association:
- 5% of adults in the United States have PTSD in a given year
- 9% of people develop it at some point in their life
Signs and symptoms of post-traumatic stress disorder can include:
- Dreams, thoughts, or feelings related to traumatic events
- Mental or physical distress to trauma-related cues
- Attempts to avoid trauma-related cues
- Shifts in how a person thinks and feels
- Increase in the fight-or-flight response
Statistically, most people who experience a traumatic event will not develop PTSD. However, some people are more susceptible to certain forms of trauma.
Women and Post-Traumatic Stress Disorder
Women are more than twice as likely to develop PTSD.
- 10% of women experience PTSD in their lifetime
- 4% of men experience PTSD in their lifetime
This is largely attributed to sexual assault because women are more likely to experience sexual assault, and sexual assault is more likely to cause PTSD than many other events. Women are also more likely to experience things like:
- Neglect or abuse in childhood
- Domestic violence
- Sudden loss of a loved one
Sadly, women may be more likely to blame themselves for their traumatic experiences than men.
When it comes to how that trauma manifests, some symptoms are more common in women. For example, women are more likely to:
- Be jumpy
- Have trouble feeling emotions
- Avoid things that remind them of trauma
- Feel depressed and anxious
Men are more likely to have issues with anger and controlling it when dealing with PTSD, but both men and women struggling with post-traumatic stress disorder can develop physical health problems.
Veterans and Post-Traumatic Stress Disorder
Of course, one portion of the population at an elevated risk of PTSD is military Veterans. According to the RAND Center for Military Health Policy Research, 20% of Veterans who served in either Iraq or Afghanistan suffer from either major depression or post-traumatic stress disorder. Combat is one of the most traumatic situations a person can be in. Witnessing death and violence, while also being exposed to life-threatening situations can easily lead to PTSD.
However, something that most people may not realize is the amount of military sexual trauma (MST) that Veterans also experience. MST is a form of sexual harassment or assault that occurs while in the military, and it happens to both men and women during training, peacetime, and in war.
According to the U.S. Department of Veteran Affairs:
- 23% of women reported sexual assault while in the military
- 55% of women in the military experience sexual harassment
- 38% of men in the military experience sexual harassment
Because there are more male Veterans than female Veterans, over half of all Veterans with military sexual trauma are actually men.
Sadly, one of the most troubling statistics about mental health when it comes to the men and women who serve our country is that according to a SAMHSA study, only around 50% of Veterans who need mental health treatment will receive it.
Post-Traumatic Stress and Substance Use Disorders
Another heartbreaking side-effect of PTSD can be drug and alcohol abuse, which often leads to substance use disorder (SUD).
In some cases, people who experience a traumatic event that causes a physical injury will be treated with powerful painkillers. This is one way that prescription opioids have contributed to the current opioid crisis in the country. Prescription opioids often increase feelings of pleasure and calm inside the brain, which can lead to those struggling with PTSD abusing these medications in order to numb themselves to both their physical agony and their emotional trauma. In fact, prescription opioid addiction is most commonly found to correlate with PTSD.
When it comes to Veterans, developing a substance use disorder with post-traumatic stress disorder is not uncommon. According to studies from the National Institute on Drug Abuse (NIDA):
- 23% of Veterans returning from Iraq or Afghanistan showed signs of SUD.
- In 2008, active duty and Veteran military personnel abused prescription drugs more than twice the rate as the civilian population.
- In 2009, the VA estimated around 13,000 Iraq and Afghanistan Veterans suffered from alcohol dependence syndrome and required mental health treatment.
Meanwhile, those who experience sexual assault are also extremely likely to turn to drugs or alcohol as a means to cope with their trauma. According to a report by the American Journal on Addictions, 75% of women who enter addiction treatment programs report having experienced sexual abuse. Many studies over the years also report a prevalence of traumatic abuse in childhood.
Ultimately, we find that PTSD can feed into substance use disorder. Many people who struggle to control their emotions and suffer from the residual effects of their experiences try to self-medicate with both legal substances and illicit narcotics.
National PTSD Awareness Month: Call for Better Treatment
For National PTSD Awareness Month we can all do our part to help raise awareness of the impact of post-traumatic stress disorder. The National Center for PTSD is urging people to:
Learn- PTSD treatment works
Connect- Reach out to someone
Share- Spread the word
Online you can get educational materials, support information and resources to help spread awareness. The National PTSD Awareness campaign encourages everyone to work together to promote effective treatment for those who are suffering.
For those struggling with PTSD and substance use disorder, Palm Healthcare Company believes in providing innovative and life-changing treatment opportunities that help people struggling with trauma and addiction to overcome adversity and build a better quality of life. Our comprehensive programs use a holistic approach to help heal the whole person, and our facilities are specially designed to create lasting change. If you or someone you love is struggling, please call toll-free now. We want to help. You are not alone.
CALL NOW 1-888-922-5398
by Justin Mckibben | Apr 18, 2018 | Addiction, Anti-Social Personality Disorder, Anxiety Disorder, Depression, Dual Diagnosis, Mental Health, Mood Disorders, Post-traumatic Stress Disorder, Schizophrenia

(This content is being used for illustrative purposes only; any person depicted in the content is a model)
It is not so far-fetched to be told that someone whose life is consumed with drug or alcohol dependency can find themselves facing the emotional and mental fallout. When dealing with mental health issues, it is not rare for people to also struggle with substance use disorder. Co-occurring conditions such as these tend to feed off of each other, or even help create one another.
It is almost like when someone has high blood pressure, we are not surprised when they develop heart problems. Sometimes side effects and symptoms of one condition can nurture new ailments.
According to so researchers, there are some more common combinations of co-occurring disorders with addictions. So which addictions are most likely to co-exist with each mental health condition?
Here are 5 of the most common co-occurring disorders with addictions (not in any particular order):
-
Schizophrenia with Marijuana Addiction

One disorder that commonly co-exists with a substance use disorder is schizophrenia. The American Journal of Psychiatry released a study that suggests approximately half of all people with schizophrenia also have a substance abuse disorder.
But one substance stands out the most when looking at people living with schizophrenia- marijuana.
The exact cause of schizophrenia is unknown, but many suspect a combination of environment, genetics and altered brain chemistry and structure to all play a part. So it is unclear why people with schizophrenia would abuse marijuana. Especially since this drug typically produces many of the same symptoms these people experience when in the midst of a schizophrenic episode. Some of these symptoms include:
- Short-term memory problems
- Delusions
- Unusual or dysfunctional ways of thinking
- Difficulty beginning and sustaining activities
- Impaired executive functioning
While not all symptoms are the same for everyone, some of these more common symptoms definitely overlap between the two. While it may not be obvious why, research suggests it is pretty obvious that marijuana is most popular for people with schizophrenia.
-
Alcoholism and Anti-Social Personality Disorder

You might be surprised with this one because most people assume alcohol is most commonly matched with depression.
Anti-social personality disorder is easier to understand when one explains the concept of personality disorders in general.
To put it simply, a personality disorder is an enduring pattern of personal experience and behavior that deviates noticeably from the expectations of the individual’s culture, which leads to personal distress of impairment. So antisocial personality disorder (ASPD) is characterized by a tendency to disregard and even violate the rights of others. Symptoms can vary from egregious to outright dangerous. They include:
- Irritability
- Aggressiveness
- Lack of remorse
- Consistent irresponsibility
- Recklessness
- Impulsivity
- Deceitfulness
- Lack of stability in a job and home life
- Disregard for society and laws
- Violation of the physical or emotional rights of others
Often the more intense cases earn the titles of sociopathic or psychopathic.
Alcohol abuse very frequency co-occurs with other mental health disorders. However, according to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), the disorder with the closest connection to alcoholism is anti-social personality disorder.
In fact, people who drink to excess on a regular basis are 21 times more likely to deal with ASPD when compared to people who don’t have alcoholism.
The NIAAA also states that both of these disorders typically develop early in life. However, alcoholism can actually make the underlying mental illness worse. Intoxication can lower an individual’s inhibitions, which makes their antisocial behaviors more prevalent. This may also lead to more dangerous manifestations of the disorder.
-
Anxiety Disorders and Cocaine Addiction

Cocaine is an extremely powerful narcotic stimulant, which gives users feelings of intense euphoria. However, the tradeoff is a very steep price to pay considering how dangerous this drug really is. Continued cocaine use typically leads to symptoms that essentially mirror an anxiety disorder, including:
- Restlessness
- Hallucinations
- Paranoia
- Insomnia
- Difficulty concentrating
- Aggression
Because cocaine is a stimulant, it speeds up and amplifies activity of the brain’s neurotransmitters. Certain neurotransmitters at higher levels induce anxiety. So anxiety is actually a symptom of cocaine use already. Cocaine use also has the potential to create psychotic episodes. Some people even experience severe mental symptoms as a result of use.
As a long-term effect of cocaine use, brain circuits are more sensitive while struggling to respond to natural stimuli, and the results are often related to mood and mental health. Statistics show that there is a very high risk of anxiety and cocaine abuse occurring together. Then if you already have an anxiety disorder, the risk becomes even higher that you will develop a severe emotional problem when using a drug like cocaine.
While the adverse effects of cocaine use can eventually fade for those able to achieve a long-lasting sobriety, sometimes the damage lingers. Those unusual thoughts and behaviors can continue even long after someone has given up the drug.
-
Prescription Opioid Addiction and PTSD

Post-traumatic stress disorder (PTSD) is a mental illness that takes hold in the aftermath of an intense and traumatic experience. Often, people who survive tragedies, war and other dangerous or life-altering events will experience PTSD.
In some circumstances, people will leave their experience with serious physical injuries, and often, those injuries are treated with prescription painkillers. This is just one way that prescription opioids have contributed to a huge epidemic that has been hurting America for the past several years.
Prescription opioids often boost feelings of pleasure and calm inside the brain, and sometimes people who have PTSD end up abusing these medications in order to experience euphoria and numb themselves to not just their physical agony, but also their emotional trauma. This can become an endless cycle of self-medicating. This is especially true with veterans. In fact, some research indicates that veterans with pain and PTSD are 3 times more likely to receive opioids compared to those without any mental health disorders.
It is true that having effective pain medications is very important to improve the quality of life for those with physical pain, especially chronic pain patients. However, mixing powerful opioids like prescription painkillers with PTSD can lead to tragic outcomes. With increasing rates of veteran suicides over the past several years, one can only image what impact the surging opioid crisis may have had on those struggling with PTSD.
-
Depression with Heroin Addiction

Throughout one of the worst drug epidemics in American history, heroin has been a driving force behind countless overdoses and skyrocketing death rates. Heroin isn’t just devastating physically, but also mentally and emotionally crippling. The connection between these adverse effects and depressive disorders is remarkable.
The allure of heroin is that is can make users feel an overwhelming sense of pleasure for a short time. However, long-time use of heroin can burn out the portions of the brain responsible for producing natural signals of pleasure, leaving them incapable of feeling good on their own without the drug. The drug alters brain chemistry and creates mood changes.
Advances in Psychiatric Treatment estimates that 48% of opioid users have experienced depression at some point in their lives.
Extended use of heroin can eventually cause a form of brain damage that leads to depression. Users can become physically incapable of feeling happiness unless the drug is present. Withdrawal symptoms from heroin can also exacerbate symptoms of depression. Many of them are actually overlapping symptoms, such as:
- Restlessness
- Irritability
- Slow thinking, speaking or body movements
- Loss of interests
- Sleep problems
- Physical pains
- Headaches
- Changes in appetite
The combination of depression and heroin addiction is incredibly common. Sometimes it can be difficult for people to tell which issue came first, but ultimately they can both be exceedingly debilitating, or even deadly.
Dual Diagnosis Treatment

Dual diagnosis means that a person is dealing with two medical conditions that are co-occurring. In regards to the field of drug addiction, dual diagnosis specifically means that someone is struggling with both substance use disorder and another mental or behavioral health issue. Sometimes it is because prolonged drug use has contributed to developing a mental health issue, while other times it is because someone has tried to self-medicate when facing a mental health issue.
Dual diagnosis treatment is so important because it provides the opportunity to treat both co-occurring disorders simultaneously. For those suffering with more than one disorder, it is not nearly as effective to focus on treating one while ignoring the other. Holistic healing is all about addressing every aspect of each individual to help them find success in every part of their life.
Palm Healthcare Company believes in providing holistic addiction resources to help treat not just the addiction, but also any other issue that could be holding you back from achieving a full life of lasting recovery. If you or someone you love is struggling, please call toll-free now.
CALL NOW 1-888-922-5398
by staff | Jan 30, 2018 | Anxiety Disorder, Coping Skills, Depression, Dual Diagnosis, Holistic Treatment, Mental Health, Mood Disorders, Post-traumatic Stress Disorder, Recovery, Self Improvement

Maintaining Mental Health and Well-Being
by Thomas G. Beley, Ph.D., LCSW
Executive Director of Palm Healthcare Company
We hear a lot about the importance of mental health. However, exactly what is mental health. If one looks at the research literature there is not very much written about what constitutes mental health. Often times, by default, mental health has been referred to or alluded to as the absence of a mental illness. To complicate the situation further, the literature seems to be overly ripe with how to treat various mental disorders as well as how to reduce the specific symptoms a person may be experiencing. Unfortunately, our society has become overly preoccupied with treatment focusing on the reduction of a person’s symptoms as an indicator of a mentally healthy person. Although treatment and symptom reduction are important facets of a person’s mental health, neither treatment nor symptom reduction guarantees a sense of well-being.
In examining the various disorders as outlined in the DSM IV and the plethora of research that has been conducted on how to treat these disorders, there appears to be a common thread that seems to exist between all of these disorders and conditions. The common thread appears to be an on-going interrelationship between the biological or neuro-chemical make-up of a person; the existing stress factors that may be presented in a person’s life; and the actually coping skills or mechanisms that a person uses as a way of dealing with everyday life. Furthermore, it appears that all three of these influences have the ability to impact the other for the better or for the worse. This article will examine these various influences on a person’s mental health and how these influences are involved in maintaining a person’s sense of mental health and well-being.
Stress
Stress is a constant in everyone’s life. Hans Selye, the father of the stress response, defined stress as “any change.” So the fact of the matter is that stress is a constant in one’s life. In essence, the moment a person opens their eyes in the morning, that’s stress. The moment that same person gets out of bed, that’s more stress. And, the moment that person jumps into the shower, even yet more stress. In most instances, our bodies are able to handle this stress much of which is attributed to a person’s balanced neurobiology and neurotransmission.
Much of this can be explained through the “fight or flight response” of a person. This mind-body connection, which has been a part of human evolution, has worked the same way over hundreds of thousands, if not millions, of years, the same way. Any time a person’s brain, either conscious or unconscious, senses any type of danger whether real or not, there are a whole host of stress hormones that are being released into the body (neurotransmission) gearing the person’s body up to do one of two things, to run away from that danger or to fight that danger. In either scenario, the body has to be an efficient machine. Although a person doesn’t necessarily have to hunt for their food any longer per se or run away from man-eating animals, a person is still faced with the everyday modern dangers of life such as unemployment, finances, marital problems, parenting, etc. The list is endless. The important point, here, is that regardless of what that perceived danger, the mind, and body via neurotransmission, kicks into action.
A problem that arises, however, is that once the mind and body have turned it up a notch to deal with the stress, it takes the body a longer time to calm down. The mind or more specifically the neocortex (the thinking part of the brain) is able to easily dismiss stress and false alarms of stress in a relatively short manner. A person can become instantly alarmed at the prospect of their electric being shut off from a notice received in the mail, however, instantly “feeling” a sense of relief realizing that the notice is not meant for them but for the neighbor. Although the mind has dismissed the danger, the stress hormones have already been released to key parts of the person’s body. Studies have shown that these stress hormones or the signaling of the mind to the body to calm down can take anywhere between six hours to seventy-two hours for the body to receive the signal of no danger. So what can actually happen is that a person can be walking around “feeling good” and the least little thing can happen, the proverbial straw that breaks the camel’s back, that can send a person into a stressed or panic state.
There are three key points that need to be remembered about stress.
The first key point is that stress is a constant in anyone’s life by virtue of the constant change a person is going through from the moment they wake up in the morning to the time they go to bed at night. All too often a person thinks of stress as “nothing bad has happened to me lately.” It is irrelevant to ask the question whether a person is stressed, it is more appropriate to think in terms of whether that person’s neurobiology is handling that stress in an appropriate manner.
Secondly, the body doesn’t really know the difference between “good stress” and “bad stress.” It may be more relevant for a person to think in terms of how much and to what extent has that person experienced change during the course of the week or the month regardless of whether that change has been “good” or “bad.” The more change the person has experienced, the more stress that has been absorbed into the body.
And, finally, the third key point is that the body is a very slow responder. It takes the body a much longer time to calm down than the cognitive processes that are occurring in the brain. A person needs to be mindful that just because they are “feeling relaxed” doesn’t necessarily mean that their body is relaxed.
It is not always feasible to assume that lowering the stressful situations in one’s life is the answer since many people may be unable to avoid a stressful lifestyle. Firefighters, police officers, emergency room medical staff, are all faced with potential chronic conditions of stress. It is not fair to say these individuals will be excluded from feeling a sense of well-being because they are in constant stressful situations. It is important for a person to be aware of trying to lower stress in their life where they can, but for those individuals who are in situations where stress is a constant, it will be more important for that person to develop the necessary coping skills to deal with stress such as exercise, nutrition, yoga, or meditation.
Neurobiology
Research in the neurosciences in recent years has continued to shed new light on a person’s brain chemistry and how neurotransmission impacts a person’s sense of well being as well as behavior. There have been numerous studies conducted on certain neurotransmitters of well being such as serotonin, GABA (gamma-aminobutyric acid), dopamine, and others to suggest the necessity of these neurotransmitters for the person to function at an optimal level. This is where the explosion of new prescription drugs has come on to the market to solve the ills of the world. Needless to say, pharmaceutical companies have long since been proponents of this neurobiological research due to the ability to develop newer and more efficient drugs to attempt to balance a person’s neurochemistry. An important aspect that has evolved over the years, however, is the recognition of, not only the importance of a person’s neurobiological chemistry to be in balance for a sense of well-being, but also the fact that a person’s biochemical makeup can be extremely delicate and subject to a whole host of outside influences such as stress, medical conditions, nutrition, and behavior that can throw a person’s neurochemistry off creating a variety of symptoms. As a result, there continues to be a growing movement toward alternative methods of treatment to address brain chemistry issues such as acupuncture, nutrition, or chiropractic intervention to intervene and/or to enhance a person’s brain chemistry.
Regardless of whether you are a proponent of Prozac or a devotee to acupuncture, the important point to emphasize is that a person’s neurochemistry plays an important role in a person’s sense of well-being and contentment. Furthermore, the imbalance of neurotransmission in the brain can interfere with that person’s overall level of functioning and well-being.
Coping
Coping with everyday life situations is another area which is an important influence on a person’s ability to achieve a sense of well-being. A person needs to feel a sense of satisfaction about how they handle given situations that confront them whether if it is with themselves or with others. However, in order to do this effectively, a person needs to have a repertoire of coping mechanisms to choose from. All too often, a person doesn’t develop or change the necessary coping skills needed to deal with life situations. An interesting point to make, here, is that the human species, which is supposed to be at the top of the so-called food chain of life, is the only species that will continue to do the exact same behaviors to problem solve a situation despite the fact that these problem-solving behaviors may have repeatedly failed in the past. For a variety of reasons, it appears that change is often difficult for a person to make. In order to effectively cope with a situation, it is of vital importance for a person to maintain a degree of flexibility, adaptation, and a willingness to change regarding any given situation.
In a sense, a person’s self-esteem can be viewed as being borne in a series of “failures.” Once a person makes a decision to do something, it is usually followed by a series of behaviors or actions. Often times these initial behaviors and actions are not going to be a success since doing something for the first time often leads to a number of miscues or possible “failures.” However, if a person is willing to persist at following through with these behaviors and actions or be willing to try something different in an attempt to reach their goal, there is a greater likelihood the person will develop a sense of competence in that area. Once that person achieves that level of competence, a person’s self-esteem will increase. Once a person’s self-esteem has increased, the easier it becomes for that person to make decisions and take action in other areas of life and the cycle begins all over again.
The important part of coping is that both coping mechanisms and skills need to be constantly reviewed and refined by a person. There is no guarantee that a particular coping skill or mechanism is going to work in all situations. As a person begins to adapt to the various complexities of life, the greater the need for a more complete range of coping skills to maintain that sense of well-being.
The Systemic Relationship of Neurobiology, Stress, and Coping
In considering these various influences on a person’s mental health and well-being, it is vital to understand the interrelationship that exists between them. One must comprehend that all three of these influences are constantly impacting one’s functioning and a person cannot focus on one of these areas without taking into consideration the ramifications it will have on the other areas. There is a cyclical force that each area has on the other areas and vice versa. For instance, if a person is experiencing an inordinate amount of stress, whether it is
“good stress” or
“bad stress,” the neurochemistry of the brain is going to be impacted. If the neurochemistry of the brain is affected, there is a greater likelihood that this imbalance is going to affect the neurotransmission which can result in symptomatic behaviors such as panic, anxiety,
depression, or other symptomatic behavior. As a result of the symptomatic behavior the person may be experiencing, the person’s coping mechanism and problem-solving abilities are probably going to be compromised at least to some degree. If the person is unable to cope with a given situation in an effective manner, there is the potential of the stress level increasing again. As a result, there is a cyclical process of impact.
Balance and Well-Being
It appears that a key factor for a person maintaining mental health and a sense of well-being is the ability to monitor and balance the areas of neurobiology, stress, and coping. The challenge, however, that confronts a person is the ability to maintain this balance on an on-going basis. One of the difficulties stems from the fact that it is not always clear as to what a person needs to attend to at any given time. For instance, let’s say that a person’s depression may simply be stemming from their genetic make-up. If this is the case, it would probably be more prudent for that person to be prescribed the appropriate anti-depressant medication to correct the neurobiological issue as opposed to getting involved in therapy or attempting to reduce stress. Although the latter two methods can be extremely effective in the long run, the more effective and efficient intervention may be from a pharmacological approach.
On the other hand, let’s say a person is depressed as a result of a great deal of existing stress that is occurring in their life, let’s say from being fired from their job, or the person has limited coping skills to deal with real-life traumas like the death of a loved one. In this scenario, a pharmacological intervention may be of little value, since the depression may be more a product of “normal” life situations that would be better addressed through support and the development of better and more appropriate coping skills for that given situation. In these situations, yoga, meditation, and exercise may be extremely efficient in addressing stressful situations whereas psychotherapy can be effective in developing better coping skills. In many instances, it is not necessarily the fact that a person’s anti-depressant or anti-anxiety medication is not working, the fact of the matter is that the person’s life is still a mess and they need to begin to put it in order. Unless the person is able to address these matters, the likelihood of a person responding effectively to a pharmacological intervention is going to be minimal.It is safe to say that one’s mental health and sense of well-being is not a given in anyone’s life. Just because a person has a positive outlook on life, doesn’t mean that their genetic make-up couldn’t play a factor in that person’s level of functioning. Or, the person who has savvy coping skills in dealing with incredible amounts of stress, doesn’t mean that the accumulative effects of those stressors will not take a physiological toll on that person via heart disease or cancer.
Maintaining mental health and well-being needs to be worked at on an on-going basis, not too different than an athlete needs to train to maintain peak performance. In the arena of mental health and well-being, a person needs to monitor and train how they are performing in the areas of neurobiology, stress reduction, and the development of more effective and positive coping skills. The ability of a person to attend to these areas through the use of yoga, nutrition, exercise, diet, meditation, stress reduction techniques, psychotherapy, hypnosis, just to name a few approaches, the greater likelihood the person will maintain that sense of well-being. A question that a person needs to ask themselves is what is it they are doing to ensure the balance of these three key areas of their life.
For over 25 year, Thomas G. Beley, PhD, LCSW has worked in the field of addictions and mental health. Over these two-and-a-half decades of helping people who struggle with mental health and substance use disorders, he has proven to be an expert clinician and innovative and compassionate leader. Palm Healthcare Company is proud to have an executive team with experience and incredible commitment to helping others. If you or someone you love is struggling, please call toll-free now. We want to help.
CALL NOW 1-888-922-5398
by Justin Mckibben | Jan 25, 2018 | Acupuncture, Addiction Medicine, Addiction Treatment, Anxiety Disorder, Holistic Treatment
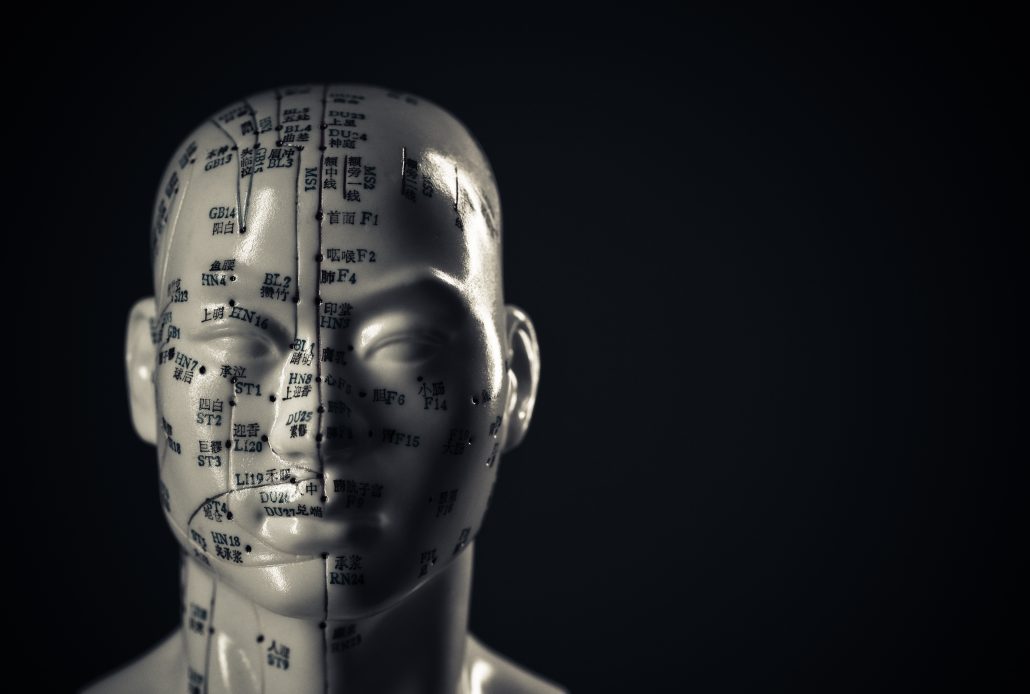
To put it simply, acupuncture is a form of alternative medicine in which thin needles are inserted into the body. This practice is a key component of traditional Chinese medicine, and the most widespread method of acupuncture in the United States derives from traditional Chinese medicine. Acupuncture therapy has been used to help heal and promote wellness for over 2,000 years.
Modern medicine explains the benefits of acupuncture using neuroscience. Traditional Chinese medicine focuses on the balance and flow of energy. Western practitioners tend to identify acupuncture points as places where stimulation to nerves, muscles, and connective tissue increases blood flow and activates the body’s natural endorphins. There are critics who say many studies on acupuncture are hard to prove because of the nature of the treatment versus control groups. Some would say any improvements may merely by placebo effects. However, many have experienced benefits from trying this method of treatment as part of personalized addiction recovery programs.
It is typical to use acupuncture for pain relief, although it can help with a wide range of other conditions as well. Generally, acupuncture is used in combination with other forms of treatment and has been known to be an effective addition to holistic addiction treatment. In 1997, the U.S. National Institute of Health (NIH) publicized acupuncture’s safety and efficacy for helping treat various conditions.
Relapse and Craving Prevention
One acupuncture technique applies small needles called “seeds” to the ear. A large study examining three auricular acupuncture protocols such as this looked at relapse prevention in drug users. This study concluded that all three protocols were associated with reductions in drug use over time.
In another study examining acupunctures impact on relapse prevention, an 8-week randomized study of 32 subjects compared two groups:
- One group was given acupuncture treatment with two prescription medications used for craving reduction
- The other received a placebo for cocaine addicts on methadone maintenance therapy
Half of the subjects in the test dropped out, so the results were not so concrete. However, almost 90% of those who completed the treatment achieved abstinence by the end of the study. The patients who completed the trial and achieved abstinence reported:
- Diminished craving
- Significantly improved mood
Over the years there have been hundreds of clinical studies on the benefits of acupuncture. According to the UC San Diego Center for Integrative Medicine, some studies claim that it can successfully help treat:
Although again, these treatments can often include medications and other forms of therapy.
Opiate Addiction and Acupuncture
The mesolimbic dopamine system originates in the ventral tegmental area (VTA) and projects to regions that include:
- Nucleus accumbens
- Prefrontal cortex
Expert believe these areas play a pivotal role in the development of opiate addiction.
Opioid abuse causes changes in the levels of dopamine in the brain. These reactions are typically associated with feelings of pleasure and well-being. This positive association helps drive the development of opiate abuse. So when someone discontinued opioid use, it reduces dopamine outflow in the nucleus accumbens. This is what creates opioid withdrawal.
Many studies in animals and humans have demonstrated that acupuncture causes multiple biological responses. The best-known mechanism is via endogenous opiates and their receptors.
In 1993, Han and Zhang reported the effectiveness of EA on morphine abstinence syndrome in a rat experimental model. The authors found that acupuncture point 100 Hz EA produced a statistically significant suppression of symptoms such as:
- Wet shakes
- Teeth chattering
- Escape attempts
- Weight loss
They also discovered acupuncture point 2 Hz EA produced a mild but significant suppression in:
- Escape attempts
- Wet shakes
These results suggest that 100 Hz EA was far more effective than 2 Hz EA in suppressing drug withdrawal syndrome. Further studies suggested that EA suppresses opiate withdrawal syndrome by activating κ opioid receptors and dynorphin release.
In short, there are researchers who believe that acupuncture is an effective method of therapy for helping treat those recovering from opioid addiction. Again, it may not be a good enough treatment on its own, but it can have an impact on cravings and other stressors in the body that help prevent relapse. So whether you believe in balancing the flow of energy in the body, or just pinpointing the nerves, acupuncture might be one way to enhance your recovery program.
Palm Healthcare Company offers acupuncture therapy as one of the many holistic treatment options to help each individual customize their own recovery plan. Acupuncture provides another opportunity to cultivate a state of physical and mental wellness in addiction recovery. Everyone struggling deserves a chance to be as healthy and happy as possible while overcoming drugs or alcohol. If you or someone you love is struggling, please call toll-free now.
CALL NOW 1-888-922-5398
by Justin Mckibben | Jan 19, 2018 | Anxiety Disorder, Coping Skills, Dual Diagnosis, Mental Health, News, Opioids, Prescription Drugs, Suicide

Over the last 15 years, the suicide rate has climbed by an estimated 32%. While the overdose deaths in relation to the opioid crisis have become a constant issue around the country, some researchers suggest that the real suicide rates are even higher, but some of them are being misclassified as overdoses.
So, are more people dying due to drug abuse, or are more people taking their own lives using powerful street drugs and prescription narcotics?
Studying Suicide and Drugs
The idea that many of the deaths recorded as opioid overdoses may have been suicides, according to the researchers, is due to a significant gap between suicide rates and intoxication mortality rates.
A study from the Luskin School of Public Affairs at the University of California, Los Angeles, was published in the journal PLOS One. This study states that both suicide and drug intoxication death rates in the United States have risen over a period of 15 years. Researchers compiled data from the Center for Disease Control and Prevention (CDC) to show:
- 2000- The suicide rate was 10.40 per 100,000 people
- 2015- Suicide rate rose to 13.75 deaths per 100,000 people
- 2000- Drug intoxication mortality rate for those over the age of 15 was 7.81 deaths per 100,000
- 2015- Drug intoxication death rate for those over the age of 15 rose to 20.07 per 100,000 in 2015
This means that the drug intoxication death rate rose by 257% in those 15 years, while suicide rates only rose by 32%. While 32% is still a devastating number when it comes to such a tragic circumstance, there is still a huge difference between 32% and 257%. These researchers believe this major difference in the reports of mortality rates suggests a lack of suicide reporting.
Difficulties in Death Investigation
One of the big problems, according to the study’s author Mark Kaplan, is resources. Kaplan is a professor of social welfare at UCLA, and he stated to local news sources,
“Unfortunately, part of the problem is due to serious under-resourcing of state and local death investigation systems throughout most of the U.S.
“Many of these deaths were probably suicides, yet reported as accidental self-poisoning rather than intentional self-harm, particularly among the middle-aged.”
The study by Kaplan and his colleagues further explains that when it comes to suicide by overdose, things like an individual’s psychiatric history or the presence of a suicide note are crucial to helping professionals identify a death as a suicide.
“A suicide note, prior suicide attempt or affective disorder was documented in less than one-third of suicides and one-quarter of undetermined deaths,”
“Our incorporation of undetermined deaths, as well as registered suicides, not only provided a window on the nature of suicide misclassification within the undetermined death category but within the accident category—as a much larger reservoir for obscuring drug intoxication suicides.”
So by acknowledging that there is not always an obvious indication that a death is a suicide, even in cases that are classified in suicide, the researchers believe that many deaths that involved drugs have most likely been categorized as overdoses instead of making a deeper inquiry into the circumstances surrounding an individual’s death.
Opioids Causing Ambiguity
With the opioid crisis in America, it has become even more difficult to measure the suicide rates. And that isn’t just this research teams opinion either.
In 2015, the CDC hosted a meeting to address the challenges presented for medical examiners and coroners across the country. The primary focus was concerning cases of fatal intoxication due to opioids and other drugs. The summary of this meeting concluded that drug intoxication deaths may be among the most difficult to determine regarding the manner of death. The summary notes that reasons for such difficulty in having a more accurate manner of death include:
- Potentially equivocal evidence
- Intent to die
- Overlapping demographic groups affected
- Overlapping premorbid risk factors (e.g., substance abuse, mental health problems).
Opioid addiction, much like any other form of substance use disorder, is often closely connected to other issues, including anxiety, trauma and mental health disorders. Some individuals living with mental health conditions who abuse opioids may be self-medicating and accidentally overdose. But others may be suffering so severely, with conditions like depressive disorders or bipolar disorder, that they ultimately take their own lives intentionally with the powerful drugs. With opioid abuse being so widespread and devastating, the line between the two has begun to blur.
Both studies mentioned clearly indicate in order to truly comprehend an accurate number of suicides by overdose, more research is needed. Both also admit that the number may never be exact.
Even though we will probably never have a definitive answer, the question is still important to ask. By knowing whether opioid deaths are caused by accidents or intentional we can develop better strategies to provide education and prevention.
This is also why mental health should always be a priority when it comes to addiction treatment.
Substance use disorder and suicide are both connected to mental health and personal wellness. Too often they both lead to avoidable tragedies. Therefore, mental health and wellness should be a priority for addiction treatment. If you or someone you love is struggling with substance abuse or addiction, please call toll-free now.
CALL NOW 1-888-922-5398
by Justin Mckibben | Oct 6, 2017 | Anxiety Disorder, Death, Depression, Dual Diagnosis, Mental Health, Mood Disorders, Prescription Drugs, Recovery

There are many national observances every month, all year round, that remind us of issues that may not always be on the forefront of our minds. These issues are typically not something everyone will put much thought into each day, but when we pause to acknowledge them for a few days at a time we may realize these are real problems that affect real people every single day. Some of these issues go unseen, like mental health disorders. One of these observances for the month of October is National Antidepressant Death Awareness Month.
If you never realized this was an actual observance, then that is kind of the point. The fact that this is enough of an issue to acknowledge for one month out of a year should speak volumes. The fact a lot of people don’t even realize it is happening says a lot too.
Let us be clear: this article is NOT to discredit or denounce the use of antidepressant medications. It is simply to acknowledge the importance of awareness and education.
So what does this observance mean?
#AntidepressantDeathAwarenessMonth
The purpose of National Antidepressant Death Awareness Month is to remember those who have been injured or killed as a result of antidepressant use. Part of this commemoration is to urge people to always report any adverse reactions while taking any drugs to the FDA, especially in cases that end in death. Depression is a common mental health disorder in the United States. In fact, recent data shows:
- More than 300 million people suffer from depression globally
- Approximately 16 million adults in the US had at least one major depressive episode in 2012
- Depression is the leading cause of disability worldwide
- 11% of adolescents have a depressive disorder by age 18
- 10%-20% of new moms will experience postpartum depression
- 30% of college students report feeling depressed enough it disrupted their performance in school
- 50% of Americans with major depression don’t seek treatment
Needless to say, depression is a prominent condition that impacts a lot of people across America. So of course, antidepressant medications are a valued resource in mental health treatment. However, excessive use of antidepressant medications or dependence on these drugs can lead to some devastating consequences.
Too often people joke about needing to “pop a Prozac” or “borrow a Zoloft” to relax, but these medications are nothing to play around with.
Antidepressants and Suicide
In 2016 reports came out about a suicide epidemic in America. According to the World Health Organization suicide was the 3rd leading cause of death in 2015, representing a 60% increase worldwide over 45 years! A report from the Center for Disease Control and Prevention (CDC) found an estimated 9.3 million adults in the United States (3.9% of the adult population) reported having suicidal thoughts in that past year.
With such shocking statistics, researchers decided to examine data on suicides and the antidepressants associated with some cases. Of most of the medications the most disturbing revelations were those for:
- Selective Serotonin Reuptake Inhibitors (SSRIs)
- Serotonin-norepinephrine Reuptake Inhibitors (SNRIs)
The review revealed that these antidepressants actually seemed to double the rate of suicide and aggressive behavior for adolescents and young people under the age of 18.
So drugs intended to treat depression actually increased risks of harmful side-effects. But even more disheartening is the fact the Big Pharma companies behind these medications were documenting “serious underestimation of the harms.” Meaning they believe drug makers misreported their findings from case studies. In many cases, researchers concluded more serious side-effects were being recorded as something else.
Side-Effects of Antidepressants
Antidepressant drugs can be very useful, but they are still drugs and should always be taken seriously. Not only can antidepressants be detrimental to emotional stability, but they cause various physical side-effects as well.
Some of the more common side-effects of antidepressants include:
- Anxiety
- Agitation
- Blurred vision
- Constipation
- Dizziness
- Nausea
- Increased appetite
- Weight gain
- Sexual dysfunction
- Fatigue
- Insomnia
- Dry mouth
- Irritability
There are other more serious health concerns that certain antidepressant drugs can contribute to as well, including:
Depending on the particular substance, some of these adverse effects of symptoms may differ. One should always speak with their doctor about the possible adverse effects of any medication and be sure to discuss all treatment options.
Be sure to consult your doctor before discontinuing any medications as well. Some of these medications can cause adverse effects when abruptly discontinued. Again, the point of this conversation is not to scare anyone away from antidepressant medications; it is simply to encourage anyone who may be taking these kinds of medications to be aware and make informed decisions with the help of your doctor.
Antidepressant Dependence
The connection between antidepressants and addiction isn’t as clear as other drugs. Doctors still debate the addictive nature of antidepressant medications, with most considering them non-addictive. However, it is possible to develop a dependence on antidepressants.
Antidepressant medications alter the brain’s chemical activity. So a lot of people use antidepressants excessively because they feel like they cannot function normally unless chemical changes in their brain activity take place. So while antidepressants may not be as addictive as other narcotic medications, people can depend on the drug to feel ‘normal’.
Antidepressant dependence commonly forms in people who never needed the drug for medical reasons. Some people receive an incorrect diagnosis of depression and thus end up on antidepressants. According to one study, doctors misdiagnosed almost 2/3 of patients with depression and prescribed unnecessary antidepressants. Still, others will abuse antidepressants for a psychostimulant-like effect.
The use of the drugs also becomes even more dangerous when combined with alcohol. People suffering from addiction to other drugs, including alcohol, also run a higher risk of abusing their antidepressants.
Combining alcohol and antidepressants can cause problems such as:
- Worsened depression or anxiety
- Intense sedation
- Dangerously high blood pressure
- Impaired coordination
- Overdose
Abuse of antidepressants can lead to overdose. Symptoms of antidepressant overdose often include:
- Impaired coordination
- Confusion
- Fainting
- Uncontrollable shaking
- Dizziness
- Irregular heartbeat
Safety before Stigma
Of course, no one should ever be afraid or embarrassed about taking an antidepressant medication. That kind of assistance can be an essential piece of someone’s balance in life, and there is no judgment.
In the realm of recovery from drug or alcohol addiction, it is important for people to understand the difficulties that others may face and accept that medical assistance might be necessary for some people to safely and comfortably grow while letting go of other dangerous substances. As long as people are willing to be mindful of how a medication effects them and take appropriate steps to protect themselves, recovery with the help of antidepressants is absolutely possible.
Approximately one in every eight adults in America take antidepressants, which are among the most commonly used medications. These medications can be life altering and important to overall health, but they must be taken seriously. This month we remember all those who have suffered through depression and been adversely affected by antidepressants. We remember those who lost their lives due to complications related to antidepressant medications, and we strive for better understanding and use of these medications to preserve lives.
Abusing prescription medications like antidepressants is extremely dangerous, and if you are trying to overcome an addiction or mental health disorder this can put you in even more danger. Getting the right kind of treatment can make all the difference. If you or someone you love is struggling, please call toll-free now.
CALL NOW 1-888-922-5398