by Justin Mckibben | Mar 28, 2019 | Addiction Medicine, Detox, Recovery, Sobriety

Physical Health is Important to Lasting Recovery
There is no doubt that substance use disorder has a dramatic impact on health. Physical, mental and emotional well-being always suffer when an individual becomes dangerously dependent on harmful substances. Drugs and alcohol have a variety of adverse effects on the body, ranging from painful withdrawal symptoms to lasting impairment of vital organs. Therefore, it should not come as a surprise that patients recovering from addiction often suffer from chronic health conditions.
Now, a new study published in the Journal of Addiction Medicine suggests that more than one-third of people recovering from addiction continue to suffer from a physical disease.
Studying Chronic Health Conditions in Addiction Recovery
Researchers from the Massachusetts General Hospital (MGH) Recovery Research Institute are the first to examine the national prevalence of medical conditions typically created or magnified by chronic and excessive use of drugs or alcohol. The data in the study comes from a nationally representative sample of more than 2,000 American adults. Each of these individuals described themselves as recovering from a range of substance issues, including:
Researchers then looked for the presence of diseases known to be exacerbated by drugs and alcohol, such as:
- Liver disease
- Diabetes
- Heart disease
- Tuberculosis
- HIV/AIDS
- Sexually transmitted infections (STIs)
- Cancer
- Hepatitis C
- Chronic obstructive pulmonary disease (COPD)
What they found was that out of all the adults recovering from substance abuse issues, 37% of them had been diagnosed with one or more of these nine conditions.
Additionally, researchers conclude that significant reductions in the participants’ quality of life connect to these conditions. Not to mention, researchers note that each of these health problems is known to reduce life expectancy.
Trends Relating to Different Drugs
When looking at the details of the data, there are a few trends that stand out. For instance, when compared to the general population, individuals in recovery have much higher levels of:
- Hepatitis C
- COPD
- Heart disease
- Diabetes
And in many cases, certain diseases more often correlate with certain substances. For example:
Hepatitis C
Rates of this condition were significantly higher for those recovering from opioids or stimulants than those recovering from alcohol.
HIV/AIDS and STIs
Lifetime prevalence of these health conditions was significantly higher in the group of people recovering from stimulant abuse than in the alcohol group.
Heart Disease
The lowest rates of this condition were actually found in individuals recovering from opioid addiction.
Diabetes
This health problem was discovered to be least common for those reporting cannabis as their primary substance issue
Multiple Chronic Conditions
The odds of experiencing two or more chronic physical diseases were increased by 4%- 7% due to certain factors, such as:
- Each additional substance used 10 times or more
- Older age at onset of diseases
- Resolving alcohol or drug problems later in life
Reduced Rates of Disease
Researchers also note a few elements that appear to coincide with reduced rates of physical diseases. In general, such factors include being:
There were also social stability and economic factors linked to lower rates of physical disease for those recovering from substance abuse, including:
- Having a household income greater than $50,000
- Higher education
- Being Employed
- Married or living with a partner
Some of these may be a bit of a surprise, especially considering that women are typically considered more susceptible to serious health problems associated with substance abuse.
Highlighting the Importance of Health in Recovery
According to the researchers, this study is important to a larger conversation about the quality of life for those in recovery from addiction. The lead and corresponding author David Eddie, Ph.D., research scientist at the Recovery Research Institute is an MGH clinical psychologist and an instructor in Psychology at Harvard Medical School. He states,
“We’ve known for a long time that chronic and heavy substance use can cause a multitude of diseases directly and indirectly – The extent to which these diseases and health conditions continue to persist for the millions of Americans who achieve recovery remains to be clarified, but this study highlights the fact that these negative impacts may continue to affect quality of life even when people achieve addiction recovery.”
Eddie believes it is important to appreciate that even those who overcome their issues with substance use disorder and drug dependence still face real physical diseases. In some cases, men and women who manage to finally make progress away from abusing drugs or alcohol still have to live the rest of their lives with other life-altering conditions. If the evidence points toward a better chance at young people and those with a shorter history of drug use being able to avoid chronic illness, then, of course, more effort should be put toward early intervention. Eddie adds,
“In addition, addiction treatment needs to be more seamlessly integrated with primary health care, and more research is needed to explore the complex relationships between alcohol and other drug use and physical disease.”
Moreover, this would further support the idea that we must address addiction as a public health issue. If we want to effectively address not only substance abuse but the long-term adverse effects of drugs and alcohol, we have to offer more comprehensive treatment options.
Part of building a healthy and effective foundation for recovery is a personalized treatment plan. Every individual is unique, and each person struggling with substance use disorder faces different challenges. That is why Palm Healthcare Company believes in providing customized and comprehensive care to every client. From medical detox resources to medication management and nutrition, we believe better health and well-being make lasting recovery possible. If you or someone you love is struggling, please call toll-free now. We want to help.
CALL NOW 1-888-922-5398
by Justin Mckibben | Jul 19, 2018 | Addiction Medicine, Drug Abuse, Maintenance Drugs, Medication-Assisted Treatment, Methadone, Naloxone, Prescription Drugs, Suboxone

The battle against opioid addiction in America is being fought every day, and many are fighting hard to create more opportunities for treatment and recovery. With more awareness being raised across the country, many are turning to medication-assisted treatment (MAT) methods as a way to address illicit opioid abuse and overdose. One of the most commonly known medications used in MAT is Suboxone.
MAT programs can be very helpful as a harm reduction strategy that gives people struggling with addiction a chance to avoid harmful withdrawals. However, addiction specialists also recognize that MAT alone is not an adequate substitute for comprehensive addiction treatment.
Furthermore, medications like Suboxone can be useful, but only to an extent. This drug may help to curb withdrawal symptoms from opioids like heroin or prescription painkillers, but it is also a powerful narcotic that can cause its own symptoms of dependence and withdrawal. Some people have tried to utilize Suboxone to get off of other drugs, only to find themselves dependent on this medication. So how do you stop using Suboxone?
More About Suboxone
Suboxone is a medication primarily for helping people stop using other opioids. The medication is a combination of two drugs:
-
Buprenorphine
Most people do not realize that Buprenorphine is itself an opioid. This semi-synthetic opioid medication is different from other opioids because it is a partial opioid agonist. What this means is that its maximal effects are less than full agonists such as heroin or methadone.
However, it still creates feelings of euphoria and respiratory depression. With chronic use, this opioid can still cause physical dependence.
-
Naloxone
This medication is used to block the effects of opioids, especially when it comes to opioid overdose. It is added to the Buprenorphine to attempt to decrease the risk of misuse. Due to the nature of this medication, if someone takes Naloxone while still experiencing the effects of an opioid it can cause them to go into sudden withdrawal.
The makers of Suboxone do warn that it can be abused in a manner similar to other opioids, both legal and illicit. They issue a number of other warnings for those considering using the medication, including:
- Injecting Suboxone may cause serious withdrawal symptoms.
- Suboxone film can cause serious, life-threatening breathing problems, overdose and death, particularly when taken intravenously in combination with benzodiazepines or other medications that act on the central nervous system.
- One should not drink alcohol while taking this medication, as it can lead to unconsciousness or even death.
Some of the adverse effects of Suboxone use include:
- Nausea
- Vomiting
- Headache
- Sweating
- Numb mouth
- Constipation
- Painful tongue
- Redness of mouth
- Intoxication
- Disturbance in attention
- Irregular heartbeat
- Sleep problems
- Blurred vision
- Back pain
- Fainting
- Dizziness
These are only a few examples. Some circumstances may lead to further complications, including someone being pregnant or living with severe hepatic impairment. You should discuss any decision you make to start or stop using Suboxone with a healthcare professional.
5 Steps to Stop Using Suboxone
-
Speak with a medical professional
If you have a Suboxone prescription, do not stop taking it without speaking to a healthcare professional first. Abruptly discontinuing a MAT program can not only cause you a great deal of discomfort, but it can be very dangerous. Trying to quit without medical assistance also creates the risk of relapse and overdose.
This is why safe medical Suboxone detox is such an important element of any addiction treatment program.
Before you decide to stop using Suboxone, speak with your personal physician or a medical addiction specialist in order to decide what is the safest and most effective way to move forward.
-
Taper vs Cold Turkey
When someone goes ‘cold turkey’ to stop using Suboxone, they essentially discontinue without any kind of medical support. Again, we remind you that this can be extremely dangerous and is always counterproductive. A better choice is to develop a plan with a medical professional that utilizes a gradual taper or even medications to assist with withdrawals.
Health experts recommend gradually reducing doses of buprenorphine. Typically, you can lower your dosage over a period of three weeks or more, reducing the doses by 10%-20% each week. The best way to decide how to do this is by working with a medical professional.
-
Get comprehensive addiction therapy
Another crucial aspect of addiction treatment is the opportunity for comprehensive addiction therapy. Individuals have a much better chance to stop using Suboxone for the long-term when they address the underlying issues that lead them to use opioids in the first place. Sometimes, drug use stems from emotional issues, trauma, or behaviors that are self-destructive. When people avoid addressing these issues, they become vulnerable to relapsing as a means to cope with them later.
Therapy not only helps people uncover the root cause of their pain, but it also teaches people new, healthy ways to cope with these issues.
-
Build a support group in recovery
Once someone has started the recovery process, a huge part of staying on the right path is to build a support group. It is very difficult to try and stop using Suboxone or any other drug all on your own. Having friends, family or mentors provides people with the resources to reach out to when they are struggling.
When trying to overcome addiction, it can be difficult for some to relate to people who do not understand addiction. Thankfully, there are support groups all over the country that offer assistance to each other while dealing with a specific issue. Most people know of 12-Step programs and other support groups for alcohol or drug addiction.
-
Participate in aftercare programs
Another useful element of treatment is aftercare. While support groups are extremely helpful, another way to stay involved in the ongoing process of addiction recovery is to get involved in aftercare programs. Many treatment providers will have programs in place to support those who have completed the inpatient levels of care, such as residential treatment, and are ready to transition back into everyday life.
When you stop using Suboxone, it is a good idea to stay connected with those who can offer support and guidance.
Understanding MAT
When a lot of people hear about medication-assisted treatment, they think it is an easy way out of addiction. Some people automatically assume that you can trade an addiction to heroin or Oxycodone for a dependence on Suboxone or another drug and everything will be fine. However, with MAT programs the goal should never be to rely on a medication for the long-term.
Medication-assisted treatment does make a difference. For some people, the fear of withdrawal symptoms keeps them using far more potent and dangerous drugs. Because they do not want to experience the pain, they keep using. Sometimes, this leads to death. So giving someone the chance to reduce the risk by using a prescription medication might keep them alive long enough to get treatment. But that is the important thing- to get the treatment.
Medications like Methadone and Suboxone are only supposed to be one piece of a more comprehensive treatment plan. They are intended to act as a short-term tool to help people ease their discomfort and avoid suffering while they try to give up drugs. MAT programs are only really effective when they are accompanied by therapy and other means of treatment. So if you want to stop using Suboxone and start recovering, seek out a rehab program that wants to help you heal.
Holistic addiction treatment is specifically designed to treat the entire person, not just the addiction. This kind of approach offers a variety of opportunities to develop new coping skills, learn more about addiction and the impact of drugs on the body, and experience innovative treatment modalities to heal the mind, body and spirit. For over 20 years, Palm Healthcare Company has been a leader in providing holistic addiction treatment. If you or someone you love is struggling, please call toll-free now.
CALL NOW 1-888-922-5398
by Justin Mckibben | May 31, 2018 | Addiction, Addiction Medicine, Addiction Stigma, Addiction Treatment, Bill Nye, Celebrity, Drug Abuse, Stigma
That quirky Science Guy with those theoretically-funky and quantifiably-fresh bow ties from your childhood is back to work making science fun with the help of celebrities and strange experiments. Since 1993, Bill Nye has been trying to teach kids, and the world, about the importance of exploring science. Now, with two seasons of his Netflix series Bill Nye Saves the World already in the bag, our boy Bill has made his way to a hard-hitting topic that has a huge impact on America today- addiction. And according to the science guy himself, one of the biggest myths he is out to debunk is that addiction is a choice. In fact, this kind of stigma may be one of the single greatest hurdles for those who need treatment.
Now we can admit that Bill Nye is not necessarily an authority on mental health or behavioral science. However, the American science communicator began his career as a mechanical engineer for Boeing Corporation, inventing a hydraulic resonance suppressor tube used on 747 airplanes. He eventually left the company to pursue a career in entertainment, and following the success of his show, Nye continued to advocate for science. He became the CEO of the Planetary Society and helped develop sundials for the Mars Exploration Rover missions. So while he may not be an expert himself, it is safe to say he is a smart man who knows how to do his research.
In a recent interview with The Fix, Bill Nye shared some of his thoughts on some of the most crucial questions we have to examine when looking at addiction and its effects. Beyond that, we look at some of the topics covered in the Netflix piece.
Bill Nye Acknowledges the Prevalence of Addiction
One of the first things Nye does is to point out how widespread the issue of addiction truly is. When asking his studio audience if they know someone living with addiction, whether in recovery or not, almost everyone in the room raised their hands. Nye tells The Fix,
“Addiction is a huge problem for our society. It’s very expensive. You have addicts getting addicted to all sorts of things and they become unproductive, they destroy their families, and they, for better or for worse, have very low qualities of life,”
Bill Nye emphasizes that addiction is not limited to a specific economic or social class, sharing a story about the wife of a close friend. This was a person who became addicted to the powerful opioid Oxycontin after breaking her ankle. This family quickly fell apart due to the addiction, despite being successful and affluent.
“It was horrible. It went on for years and years…she got into harder and harder drugs. She was an accessory to murder with a drug dealer, and this was a family that was very well off because of their success and careers. It was really heartbreaking.”
Throughout the segments, Bill Nye continues to expand on the brain’s involvement in addiction. He even bring in people to discuss treatments, and talks about behavioral addictions.
Addressing Choice and Changes in the Brain
Early on in “The Addiction Episode” of Bill Nye Saves the World, the science guy makes a point to distinguish from “really liking chocolate or re-watching episodes of Game of Thrones” and “real conditions that do real harm.”
He immediately points out that our society often believes addiction is an obvious choice, an avoidable weakness, or a moral failure. If you have been awake for the past few decades, you have probably seen this opinion expressed at some point. From lengthy articles like this one (but with better writers) to viral videos on social media featuring some guy yelling at a camera phone because it makes him an expert, people have argued that if people were strong enough they would fix themselves. Bill Nye says,
“I’m here to tell you that just ain’t so.”
Now, while Bill Nye may not be an addiction expert himself, he has surely done his homework over the years by interviewing various experts in the field of addiction medicine and recovery. This isn’t even the first time he’s tried to debunk the myth of addiction being a choice. Years ago he did a similar episode addressing addiction on the show The Eyes of Nye, which featured addictionologist, Dr. Drew. In this past interview, Dr. Drew makes a very strong argument stating:
“The definition of a disease, to me, would be an abnormal physiological process brought on by a relationship between the genetics of the individual and the environment that creates a set of signs and symptoms that progress in a predictable way which we call ‘natural history,’ and by effecting the natural history we can create a predictable response to treatment. That is a disease, and addiction does fit that.”
On Bill Nye Saves the World, he uses his trademark fun and goofy way to explain how dopamine released in the brain’s reward center by particular behaviors over time actually changes the brain, with the help of orange trees and a light-up LED brain. Nye states,
“When and if this happens depends on both the hand you are dealt- your genes- and what’s going on around you- your environment- it’s akin to the old question of nature versus nurture. Except with addiction, it’s both. It’s nature… and nurture!”
Bill Nye explains later on how the human ability to adapt is intimately connected to addiction, adding that while we can get used to just about anything when our brains and bodies adapt to a drug it makes quitting incredibly difficult to accomplish, especially when you factor in withdrawal symptoms.
Putting Addiction into Perspective
But good old Bill doesn’t expect you to just take his word for it, either. Throughout the episode he speaks with various people concerning the truth about addiction and different kinds of treatment for addiction. The conversations include people with various points of reference, including:
-
Maria Bamford, comedian/actress
Bamford sits with Bill to discuss her own experience with what she calls an “addictive process”: an eating disorder. She talks about finding a 12-Step program at 21 years old, and the value she has found in connecting with others.
-
Cara Santa Maria, science communicator and journalist
Cara Santa Maria talks about the importance of having individualized treatment options that go above and beyond the traditional 12 step programs. She also believes that people should also consider connecting addiction to deeper psychological issues, such as trauma.
Dr. Carl Hart advocates that there is a real need for more comprehensive assessments concerning addiction. Dr. Hart believes the vast majority of people who use drugs, including heroin, do not become addicted. Dr. Hart believes also putting too much focus on the drugs and not enough focus on the behaviors makes treatment less effective.
-
Lieutenant Robert Chromik Jr. of a Sherriff’s Office in Ohio
The officer from Ohio states that his precinct has been working to help people get clean instead of arresting them. He says that out of 2,400 “clients” involved in the program, 81% are now living clean. Lt. Chromik also agrees with his fellow panelists that specialized treatment is essential because there is no one-size-fits-all answer.
In the end, the episode is pretty interesting. This writers only critque would be that the ending itself seems almost incomplete. It includes an unrelated, but pretty cool segment about aquaculture with a guest scientist. Still, without a definitive signing-off moment to summarize the concepts Bill covers, the impact of a scientific understanding of addiction almost feels lost. However, between the piece from The Eyes of Nye and this new episode, there is a lot of interesting information that is essential to our society learning to treat addiction, and those who are suffering, better. Overall, one of the most important parts of the conversation is the emphasis on compassion and supporting effective and individualized treatment options. Bill Nye and the many individuals throughout the episode present various perspectives on the issue of addiction. Surely, not all these people agree on everything. Still, the episode works hard to offer a simple explanation of the scientific evidence in the brain and the body as to how addiction really works. Hopefully, more people can appreciate the science behind it.
Thanks Bill. Science still rules.
Another important take away from this episode is that personalized treatment is a unique and life-changing tool to helping get people off of drugs or alcohol. If you or someone you love is struggling, there is professional and innovative help for you today. Please call toll-free now.
CALL NOW 1-888-922-5398
by Justin Mckibben | Jan 25, 2018 | Acupuncture, Addiction Medicine, Addiction Treatment, Anxiety Disorder, Holistic Treatment
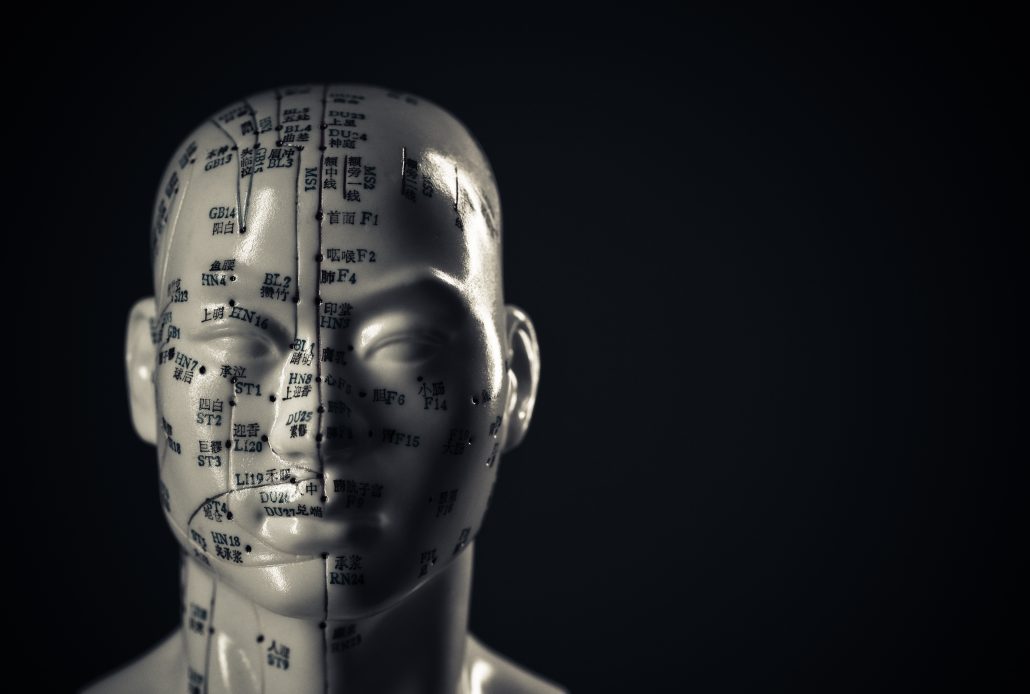
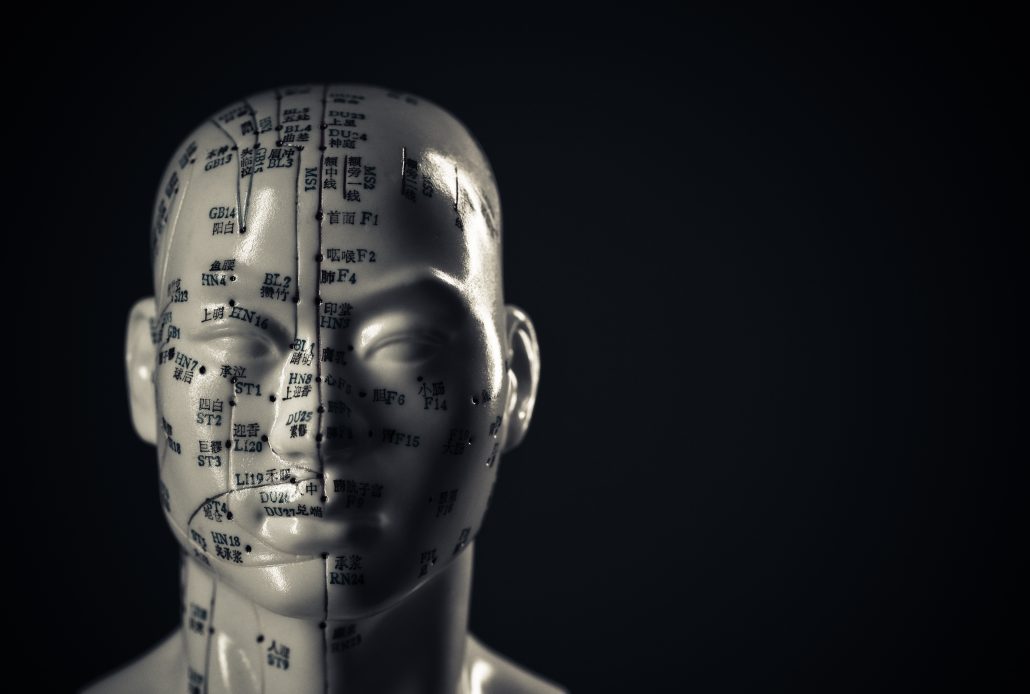
To put it simply, acupuncture is a form of alternative medicine in which thin needles are inserted into the body. This practice is a key component of traditional Chinese medicine, and the most widespread method of acupuncture in the United States derives from traditional Chinese medicine. Acupuncture therapy has been used to help heal and promote wellness for over 2,000 years.
Modern medicine explains the benefits of acupuncture using neuroscience. Traditional Chinese medicine focuses on the balance and flow of energy. Western practitioners tend to identify acupuncture points as places where stimulation to nerves, muscles, and connective tissue increases blood flow and activates the body’s natural endorphins. There are critics who say many studies on acupuncture are hard to prove because of the nature of the treatment versus control groups. Some would say any improvements may merely by placebo effects. However, many have experienced benefits from trying this method of treatment as part of personalized addiction recovery programs.
It is typical to use acupuncture for pain relief, although it can help with a wide range of other conditions as well. Generally, acupuncture is used in combination with other forms of treatment and has been known to be an effective addition to holistic addiction treatment. In 1997, the U.S. National Institute of Health (NIH) publicized acupuncture’s safety and efficacy for helping treat various conditions.
Relapse and Craving Prevention
One acupuncture technique applies small needles called “seeds” to the ear. A large study examining three auricular acupuncture protocols such as this looked at relapse prevention in drug users. This study concluded that all three protocols were associated with reductions in drug use over time.
In another study examining acupunctures impact on relapse prevention, an 8-week randomized study of 32 subjects compared two groups:
- One group was given acupuncture treatment with two prescription medications used for craving reduction
- The other received a placebo for cocaine addicts on methadone maintenance therapy
Half of the subjects in the test dropped out, so the results were not so concrete. However, almost 90% of those who completed the treatment achieved abstinence by the end of the study. The patients who completed the trial and achieved abstinence reported:
- Diminished craving
- Significantly improved mood
Over the years there have been hundreds of clinical studies on the benefits of acupuncture. According to the UC San Diego Center for Integrative Medicine, some studies claim that it can successfully help treat:
Although again, these treatments can often include medications and other forms of therapy.
Opiate Addiction and Acupuncture
The mesolimbic dopamine system originates in the ventral tegmental area (VTA) and projects to regions that include:
- Nucleus accumbens
- Prefrontal cortex
Expert believe these areas play a pivotal role in the development of opiate addiction.
Opioid abuse causes changes in the levels of dopamine in the brain. These reactions are typically associated with feelings of pleasure and well-being. This positive association helps drive the development of opiate abuse. So when someone discontinued opioid use, it reduces dopamine outflow in the nucleus accumbens. This is what creates opioid withdrawal.
Many studies in animals and humans have demonstrated that acupuncture causes multiple biological responses. The best-known mechanism is via endogenous opiates and their receptors.
In 1993, Han and Zhang reported the effectiveness of EA on morphine abstinence syndrome in a rat experimental model. The authors found that acupuncture point 100 Hz EA produced a statistically significant suppression of symptoms such as:
- Wet shakes
- Teeth chattering
- Escape attempts
- Weight loss
They also discovered acupuncture point 2 Hz EA produced a mild but significant suppression in:
- Escape attempts
- Wet shakes
These results suggest that 100 Hz EA was far more effective than 2 Hz EA in suppressing drug withdrawal syndrome. Further studies suggested that EA suppresses opiate withdrawal syndrome by activating κ opioid receptors and dynorphin release.
In short, there are researchers who believe that acupuncture is an effective method of therapy for helping treat those recovering from opioid addiction. Again, it may not be a good enough treatment on its own, but it can have an impact on cravings and other stressors in the body that help prevent relapse. So whether you believe in balancing the flow of energy in the body, or just pinpointing the nerves, acupuncture might be one way to enhance your recovery program.
Palm Healthcare Company offers acupuncture therapy as one of the many holistic treatment options to help each individual customize their own recovery plan. Acupuncture provides another opportunity to cultivate a state of physical and mental wellness in addiction recovery. Everyone struggling deserves a chance to be as healthy and happy as possible while overcoming drugs or alcohol. If you or someone you love is struggling, please call toll-free now.
CALL NOW 1-888-922-5398
by staff | Nov 24, 2017 | Addiction Medicine, Addiction Treatment, Maintenance Drugs, Medication-Assisted Treatment, Methadone, Prescription Drugs, Recovery, Suboxone, Vivitrol

Support for Medication-Assisted Treatment (MAT) has continued to grow in recent years as the opioid epidemic in America has put a mounting strain on the country. While the numbers of overdoses and opioid-related deaths have steadily climbed to devastating heights there has been more effort to explore treatment options. A better understanding of the medical and mental health aspects of addiction has become a priority. Stigma has slowly begun to carry less weight while advocates push for more effective and supportive routes to care for recovering addicts. One thing people have turned to heavily is medications like Suboxone of Methadone in attempts to steer away from more illicit and dangerous substances like heroin or fentanyl.
The application of medication in treatment can be very useful. It is a strategy that can help with the preservation of life by helping people stay off more unpredictable and life-threatening substances. However, some would say that if used for long-term this form of treatment is still relying on the idea of substitution. Often times these drugs have their own very harsh withdrawal symptoms, especially with extended use.
Taking a look at the more popular drugs used for medication-assisted treatment, one may ask- can you quit medication-assisted treatment with no withdrawals?
Understanding Medication-Assisted Treatment
Medication Assisted Treatment is the use of anti-craving medications to try and help address issues related to drug dependence, withdrawal, and relapse. The more common medications used in MAT include:
But MAT is also utilized alongside comprehensive therapy and other forms of support. Experts and advocates for addiction recovery, including the Substance Abuse and Mental Health Services Administration (SAMHSA), insist that maintenance medications alone are not sufficient enough treatment.
Advocates for medication-assisted treatment will compare MAT to someone taking medication for diabetes or asthma, with the belief that maintenance drugs are an essential part of staying healthy. However, others in the world of addiction recovery still believe it is possible to be healthy in recovery without the prolonged use of powerful medications.
The truth is the answer may not be the same for everybody. Different treatments may be more useful for different people. No one should be ashamed of the method they use to get help. But we also want to look at how some drugs used in medication-assisted treatment might make things more complicated for certain people.
Suboxone
Looking at the most popular maintenance drugs for opioid addiction, of course, we find Suboxone. To better understand Suboxone withdrawals, we first have to know what it is. This popular brand name is used to identify a prescription medication that contains active ingredients:
- Buprenorphine- a narcotic opioid medication
- Naloxone– an opioid blocker that impedes the effect of opioid medications
This medication functions as a partial opioid agonist and diminishes cravings as well as prevents other opioids from reacting to the brain’s opioid receptors. Taken in low doses for short periods of time, the drug can be helpful in curbing opioid withdrawal symptoms while tapering off without too many residual effects.
The tricky part comes when someone uses Suboxone for an extended amount of time as a replacement for heroin or other opioids.
Sometimes this can lead to its own form of recreational use and physical dependence. Even the U.S. Drug Enforcement Administration reports that Suboxone is commonly susceptible to abuse. It is still a powerful drug.
Suboxone Withdrawal Symptoms
While Suboxone and other maintenance drugs may be a preferred tactic for going ‘cold turkey’ off of heroin or other opioids, the drug itself still has the power to cause its own set of withdrawal symptoms. These symptoms can include:
- Irritability or agitation
- Anxiety
- Difficulty sleeping
- Profuse sweating
- Tearing
- Runny nose
- Frequent yawning
- Stomach pain or cramping
- Diarrhea
- Dilated pupils
- Nausea and vomiting
- Confusion
- Changes in mood
Not to mention precipitated withdrawal, when the ingredients in this medication can actually induce the onset of unpleasant symptoms rapidly, if not immediately, for someone actively engaged in opioid use.
Methadone
Methadone is a long-acting opioid medication utilized since the 1970s to try and help people get off of heroin. It is typically used today under strict medical supervision because the drug is very potent and has a high risk of addiction. In fact, a 2012 National Survey on Drug Use and Health found that approximately 2.46 million people reported to using methadone for a non-prescribed purpose at least once.
According to another study, in 2009 methadone was responsible for 1 out of every 3 opioid overdose deaths.
Because of the risks, a gradual taper should be utilized to wean someone off of methadone. Often times doctors will prescribe another detox medication to help with this process, with the tapering to be done under medical supervision.
Methadone Withdrawal
But as with trying to quit heroin or other powerful opioids ‘cold turkey’, trying to abruptly discontinue methadone can bring on intense withdrawal. This includes physical and psychological symptoms such as:
- Agitation
- Anxiety
- Depression
- Insomnia
- Runny nose
- Tearing or watery eyes
- Muscle aches
- Joint pain
- Sweating
- Nausea
- Abdominal cramps
- Diarrhea
- Vomiting
- Shivering
- Trembling
Many of these symptoms are similar to the symptoms of withdrawing from heroin or other opioids. So in a sense, this drug can create similar withdrawal symptoms as the drugs it is supposed to be used to treat.
Quitting Medication Assisted Treatment
Is it possible to quit medication-assisted treatment- yes, there are always other options for getting comprehensive care and lasting recovery without the prolonged use of these medications. Even relapse prevention is possible without relying on medications to fight cravings.
Can you quit medication-assisted treatment with no withdrawals? Well, that may be a process. It depends on a number of factors, such as the specific maintenance medication and the length of time using it. For example, someone who has been using methadone for years could probably have a much harder time getting off methadone than someone who used another medication for a month or so to help get off opioids.
Safety is crucial when deciding to quit MAT. Quitting medication-assisted treatment without a taper or other forms of medication can cause intense withdrawals. It is not suggested that someone try to quit MAT ‘cold turkey’ or without consulting a doctor for help with changing the dosage and slowly tapering off the drugs.
Again, just because it isn’t heroin or fentanyl doesn’t make it harmless.
MAT or Detox?
Medication-assisted treatment holds a lot of value, but the question becomes whether or not it is the kind of sustainable solution you want. Recovery isn’t one-size-fits-all. Medication-assisted treatment can be helpful in saving someone’s life who cannot stop using drugs. But is it something that will completely eliminate cravings and withdrawals, or will it just postpone these symptoms?
Remember, these are still powerful narcotic drugs that have a high risk for abuse. Some people end up using medication maintenance for life. Others will use it for a short period of time, with a detox period afterward. Either way, it is your choice; how long do you want to rely on substances, and to what extent?
Other models believe in providing holistic treatment and personalized therapy after a detox period, helping to reduce and remove chemical dependence and build a foundation for personal recovery.
Using medication to help with the painful and often overwhelming symptoms of withdrawal from opioids and other drugs can be essential to a smooth and healthy transition. In fact, with a safe medical detox, each individual is given an initial assessment to see what medications will be helpful in making this phase of treatment comfortable and safe. This can include medications for anxiety, mood disorders, physical pains and various other side-effects of substance abuse.
And when it comes to some of these medications, it can sometimes be necessary to continue using them.
The biggest difference is whether narcotic maintenance medications like Suboxone or methadone become a long-term prerequisite to recovery, or if they are used to help someone who is sick get better so that the real healing can happen.
Palm Healthcare Company believes in providing a safe medical detox to allow for a comfortable and healthy transition from active drug or alcohol use. Our facilities utilize an experienced and professional medical staff who help to monitor each individual’s progress and provide effective medical support for lasting recovery. If you or someone you love is struggling with substance abuse or addiction, please call toll-free now. We want to help.
CALL NOW 1-888-922-5398
by Justin Mckibben | Oct 9, 2017 | Addiction Medicine, Alcohol Addiction, Detox, Nutraceutical Therapy

Recently I heard about a new product making a little noise online for being advertised as an all-natural supplement used for drug detox. I had never heard of Mitadone before, but I had heard about people trying to promote what they call more natural home remedies for treating withdrawal symptoms. Some claim to use natural juice cleansing regiments, or synthetic herbal compounds, or various other forms of healthy dietary routines to assist in their recovery from drug or alcohol addiction. However, it seems some people are looking to Mitadone as some kind of ‘miracle supplement.’
So what is Mitadone? Does it Work?
Mitadone Detox
When visiting the official website for Mitadone, one of the first things you will see is that the company claims to offer a variety of detox programs, including:
Some of these options have a number of supplement plans, with different combinations of supplements which seem to imply they assist with different functions at different stages.
For Example- the Opiate Aid Program has a 3 step program with:
- Opiate Withdrawal Aid- 120 Tablets
- 5 Day Detox- 60 Capsules
- Anxiety, Stress Relief, and Mood Support- 90 Capsules
Each with a different purpose and including different ingredients. So what kind of all-natural ingredients are there?
Anit-Opiate Aid Plus Extra Strength
This product is advertised on the site as helping with withdrawal symptoms and cravings from opioid medications and illicit opioids like heroin. The ingredients are listed as:
- Vitamin A (as Beta Carotene)
- Biotin
- Vitamin C (as Ascorbic Acid)
- Calcium
- Vitamin D3 (as Cholecalciferol)
- Pantothenic Acid
- Vitamin E (as D-Alpha Tocopheryl Succinate)
- Glutathione
- Vitamin K1
- Kudzu Root
- Vitamin B1
- Vitamin B2
- Niacin
- Vitamin B6
- Folic Acid
- Vitamin B12
- Magnesium
- L-Theanine
- Guarana
- CoQ10
- 5-HTP
- SAM-e
- Melatonin
- John’s Wort
- L-Arginine
- Rutin Bioperine
- Ginger
- Turmeric
- Peppermint
- Dicalcium Phosphate
- Microcrystalline Cellulose
- Croscarmellose Sodium
- Stearic Acid
- Vegetable Stearate
- Silicon Dioxide
- Pharmaceutical Glaze
Quite a mouth-full, right?
Oh and guess what- its Gluten Free!
The site states the product is “manufactured by a GMP (Good Manufacturing Practices) approved facility that employs FDA certified manufacturing and quality control procedures.” Essentially, the Mitadone program is a large supply of multi-vitamins and other supplements. There are no prescription chemicals or habit-forming substances, according to their description.
Does it Work?
So are these multi-vitamin routines enough to combat such powerful addictions as opioids or alcohol? Well, Mitadone claims with their products you can detox from home, but is that really safe?
With alcohol detox, some withdrawal symptoms can be particularly harmful to your body. Others can even be lethal. With opioids, withdrawals can be extremely uncomfortable or even painful. So while these supplements may be able to help supply nutrients to the body, they aren’t exactly going to be able to support every aspect of the detox process.
If you look closer at the descriptions of these products, it seems Mitadone also knows how limited its impact can be. The fine-print acknowledges that everyone’s body chemistry is different, so the supplements will not always affect everyone the same. Some of the better reviews on Amazon.com still say that while the supplements made them feel a little better in some aspects, they were still extremely sick. Others claim the supplements did nothing to ease the more severe symptoms of opioid withdrawal.
When looking into the product and reading reviews, it is often but in the same category as Kava, which is a beverage or extract that is often advertised as a more natural substance. Some use Kava for recreational purposes. Others also use Kava to try and fight their withdrawals. If we look closer at Kava, it has much of its own controversy. There is a lot of contention as to whether Kava is responsible for liver damage and other health risks. While Mitadone is a totally different product, people associate them both with the concept of self-detoxing through ‘natural remedies’. Yet, many still question how safe or effective they are.
Even on the Mitadone website, in the Opiate Aid and Alcohol Aid programs you can see statements like:
“Increases the chances of substance abuse patients to stay in any maintenance therapy program.”
“Addiction doesn’t necessarily conclude after the patient exits a rehab program.”
So even in their product descriptions, they seem to admit that these supplements are not a solution on their own, but a product that might give someone a better chance while pursuing other specific treatment options.
In short, these kinds of nutritional products can be an asset to your recovery plan, but they are ineffective as a primary recovery strategy.
Nutraceutical Therapy and Addiction Treatment
Incorporating a healthier diet and perhaps even vitamins and other supplements can be very beneficial for some, but they should be utilized as part of a more holistic approach to addiction recovery.
Palm Healthcare Company offers Nutraceutical Therapy as part of a holistic addiction treatment program. We understand the importance of nourishing the body while also healing the mind. The value of vitamin and supplement therapy should not be underestimated. There is a benefit to supplements such as:
- Multivitamins
- Probiotics
- Digestive enzymes
- Phytonutrients
- Essential fatty acids
Combine these with a healthy, balanced diet and physical therapy can provide an exceptional advantage to someone on the path to recovery.
But we emphasize that recovering from addiction to drugs or alcohol is not just about balancing out the body to help it break its dependence on substances. Recovery is also about comprehensive addiction education, developing new coping skills and addressing personal traumas. There is so much more to a future in recovery.
Mitadone may have a decent product, but people should always remember that with drug addiction it is not always effective, or even safe, to detox on your own. Medical detox is a resource that exists to help people get off drugs as safely and effectively as possible, while providing various lines of support, including nutrition.
Nutritional therapy in addiction treatment recognizes the importance of what we put into our bodies, but it is most effective as part of a complete treatment plan. For those trying to find ways to overcome withdrawal symptoms, a medical detox with experienced professionals can make the process safer and easier. If you or someone you love is struggling, please call toll-free now.
CALL NOW 1-888-922-5398