by staff | Jan 30, 2018 | Anxiety Disorder, Coping Skills, Depression, Dual Diagnosis, Holistic Treatment, Mental Health, Mood Disorders, Post-traumatic Stress Disorder, Recovery, Self Improvement

Maintaining Mental Health and Well-Being
by Thomas G. Beley, Ph.D., LCSW
Executive Director of Palm Healthcare Company
We hear a lot about the importance of mental health. However, exactly what is mental health. If one looks at the research literature there is not very much written about what constitutes mental health. Often times, by default, mental health has been referred to or alluded to as the absence of a mental illness. To complicate the situation further, the literature seems to be overly ripe with how to treat various mental disorders as well as how to reduce the specific symptoms a person may be experiencing. Unfortunately, our society has become overly preoccupied with treatment focusing on the reduction of a person’s symptoms as an indicator of a mentally healthy person. Although treatment and symptom reduction are important facets of a person’s mental health, neither treatment nor symptom reduction guarantees a sense of well-being.
In examining the various disorders as outlined in the DSM IV and the plethora of research that has been conducted on how to treat these disorders, there appears to be a common thread that seems to exist between all of these disorders and conditions. The common thread appears to be an on-going interrelationship between the biological or neuro-chemical make-up of a person; the existing stress factors that may be presented in a person’s life; and the actually coping skills or mechanisms that a person uses as a way of dealing with everyday life. Furthermore, it appears that all three of these influences have the ability to impact the other for the better or for the worse. This article will examine these various influences on a person’s mental health and how these influences are involved in maintaining a person’s sense of mental health and well-being.
Stress
Stress is a constant in everyone’s life. Hans Selye, the father of the stress response, defined stress as “any change.” So the fact of the matter is that stress is a constant in one’s life. In essence, the moment a person opens their eyes in the morning, that’s stress. The moment that same person gets out of bed, that’s more stress. And, the moment that person jumps into the shower, even yet more stress. In most instances, our bodies are able to handle this stress much of which is attributed to a person’s balanced neurobiology and neurotransmission.
Much of this can be explained through the “fight or flight response” of a person. This mind-body connection, which has been a part of human evolution, has worked the same way over hundreds of thousands, if not millions, of years, the same way. Any time a person’s brain, either conscious or unconscious, senses any type of danger whether real or not, there are a whole host of stress hormones that are being released into the body (neurotransmission) gearing the person’s body up to do one of two things, to run away from that danger or to fight that danger. In either scenario, the body has to be an efficient machine. Although a person doesn’t necessarily have to hunt for their food any longer per se or run away from man-eating animals, a person is still faced with the everyday modern dangers of life such as unemployment, finances, marital problems, parenting, etc. The list is endless. The important point, here, is that regardless of what that perceived danger, the mind, and body via neurotransmission, kicks into action.
A problem that arises, however, is that once the mind and body have turned it up a notch to deal with the stress, it takes the body a longer time to calm down. The mind or more specifically the neocortex (the thinking part of the brain) is able to easily dismiss stress and false alarms of stress in a relatively short manner. A person can become instantly alarmed at the prospect of their electric being shut off from a notice received in the mail, however, instantly “feeling” a sense of relief realizing that the notice is not meant for them but for the neighbor. Although the mind has dismissed the danger, the stress hormones have already been released to key parts of the person’s body. Studies have shown that these stress hormones or the signaling of the mind to the body to calm down can take anywhere between six hours to seventy-two hours for the body to receive the signal of no danger. So what can actually happen is that a person can be walking around “feeling good” and the least little thing can happen, the proverbial straw that breaks the camel’s back, that can send a person into a stressed or panic state.
There are three key points that need to be remembered about stress.
The first key point is that stress is a constant in anyone’s life by virtue of the constant change a person is going through from the moment they wake up in the morning to the time they go to bed at night. All too often a person thinks of stress as “nothing bad has happened to me lately.” It is irrelevant to ask the question whether a person is stressed, it is more appropriate to think in terms of whether that person’s neurobiology is handling that stress in an appropriate manner.
Secondly, the body doesn’t really know the difference between “good stress” and “bad stress.” It may be more relevant for a person to think in terms of how much and to what extent has that person experienced change during the course of the week or the month regardless of whether that change has been “good” or “bad.” The more change the person has experienced, the more stress that has been absorbed into the body.
And, finally, the third key point is that the body is a very slow responder. It takes the body a much longer time to calm down than the cognitive processes that are occurring in the brain. A person needs to be mindful that just because they are “feeling relaxed” doesn’t necessarily mean that their body is relaxed.
It is not always feasible to assume that lowering the stressful situations in one’s life is the answer since many people may be unable to avoid a stressful lifestyle. Firefighters, police officers, emergency room medical staff, are all faced with potential chronic conditions of stress. It is not fair to say these individuals will be excluded from feeling a sense of well-being because they are in constant stressful situations. It is important for a person to be aware of trying to lower stress in their life where they can, but for those individuals who are in situations where stress is a constant, it will be more important for that person to develop the necessary coping skills to deal with stress such as exercise, nutrition, yoga, or meditation.
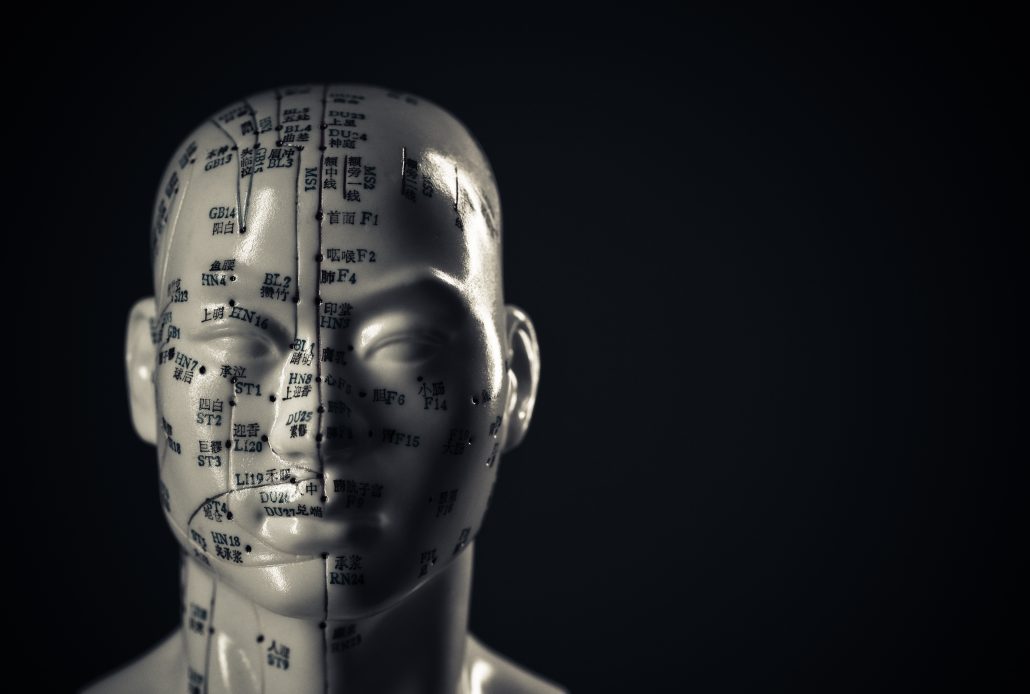
Neurobiology
Research in the neurosciences in recent years has continued to shed new light on a person’s brain chemistry and how neurotransmission impacts a person’s sense of well being as well as behavior. There have been numerous studies conducted on certain neurotransmitters of well being such as serotonin, GABA (gamma-aminobutyric acid), dopamine, and others to suggest the necessity of these neurotransmitters for the person to function at an optimal level. This is where the explosion of new prescription drugs has come on to the market to solve the ills of the world. Needless to say, pharmaceutical companies have long since been proponents of this neurobiological research due to the ability to develop newer and more efficient drugs to attempt to balance a person’s neurochemistry. An important aspect that has evolved over the years, however, is the recognition of, not only the importance of a person’s neurobiological chemistry to be in balance for a sense of well-being, but also the fact that a person’s biochemical makeup can be extremely delicate and subject to a whole host of outside influences such as stress, medical conditions, nutrition, and behavior that can throw a person’s neurochemistry off creating a variety of symptoms. As a result, there continues to be a growing movement toward alternative methods of treatment to address brain chemistry issues such as acupuncture, nutrition, or chiropractic intervention to intervene and/or to enhance a person’s brain chemistry.
Regardless of whether you are a proponent of Prozac or a devotee to acupuncture, the important point to emphasize is that a person’s neurochemistry plays an important role in a person’s sense of well-being and contentment. Furthermore, the imbalance of neurotransmission in the brain can interfere with that person’s overall level of functioning and well-being.
Coping
Coping with everyday life situations is another area which is an important influence on a person’s ability to achieve a sense of well-being. A person needs to feel a sense of satisfaction about how they handle given situations that confront them whether if it is with themselves or with others. However, in order to do this effectively, a person needs to have a repertoire of coping mechanisms to choose from. All too often, a person doesn’t develop or change the necessary coping skills needed to deal with life situations. An interesting point to make, here, is that the human species, which is supposed to be at the top of the so-called food chain of life, is the only species that will continue to do the exact same behaviors to problem solve a situation despite the fact that these problem-solving behaviors may have repeatedly failed in the past. For a variety of reasons, it appears that change is often difficult for a person to make. In order to effectively cope with a situation, it is of vital importance for a person to maintain a degree of flexibility, adaptation, and a willingness to change regarding any given situation.
In a sense, a person’s self-esteem can be viewed as being borne in a series of “failures.” Once a person makes a decision to do something, it is usually followed by a series of behaviors or actions. Often times these initial behaviors and actions are not going to be a success since doing something for the first time often leads to a number of miscues or possible “failures.” However, if a person is willing to persist at following through with these behaviors and actions or be willing to try something different in an attempt to reach their goal, there is a greater likelihood the person will develop a sense of competence in that area. Once that person achieves that level of competence, a person’s self-esteem will increase. Once a person’s self-esteem has increased, the easier it becomes for that person to make decisions and take action in other areas of life and the cycle begins all over again.
The important part of coping is that both coping mechanisms and skills need to be constantly reviewed and refined by a person. There is no guarantee that a particular coping skill or mechanism is going to work in all situations. As a person begins to adapt to the various complexities of life, the greater the need for a more complete range of coping skills to maintain that sense of well-being.
The Systemic Relationship of Neurobiology, Stress, and Coping
In considering these various influences on a person’s mental health and well-being, it is vital to understand the interrelationship that exists between them. One must comprehend that all three of these influences are constantly impacting one’s functioning and a person cannot focus on one of these areas without taking into consideration the ramifications it will have on the other areas. There is a cyclical force that each area has on the other areas and vice versa. For instance, if a person is experiencing an inordinate amount of stress, whether it is
“good stress” or
“bad stress,” the neurochemistry of the brain is going to be impacted. If the neurochemistry of the brain is affected, there is a greater likelihood that this imbalance is going to affect the neurotransmission which can result in symptomatic behaviors such as panic, anxiety,
depression, or other symptomatic behavior. As a result of the symptomatic behavior the person may be experiencing, the person’s coping mechanism and problem-solving abilities are probably going to be compromised at least to some degree. If the person is unable to cope with a given situation in an effective manner, there is the potential of the stress level increasing again. As a result, there is a cyclical process of impact.
Balance and Well-Being
It appears that a key factor for a person maintaining mental health and a sense of well-being is the ability to monitor and balance the areas of neurobiology, stress, and coping. The challenge, however, that confronts a person is the ability to maintain this balance on an on-going basis. One of the difficulties stems from the fact that it is not always clear as to what a person needs to attend to at any given time. For instance, let’s say that a person’s depression may simply be stemming from their genetic make-up. If this is the case, it would probably be more prudent for that person to be prescribed the appropriate anti-depressant medication to correct the neurobiological issue as opposed to getting involved in therapy or attempting to reduce stress. Although the latter two methods can be extremely effective in the long run, the more effective and efficient intervention may be from a pharmacological approach.
On the other hand, let’s say a person is depressed as a result of a great deal of existing stress that is occurring in their life, let’s say from being fired from their job, or the person has limited coping skills to deal with real-life traumas like the death of a loved one. In this scenario, a pharmacological intervention may be of little value, since the depression may be more a product of “normal” life situations that would be better addressed through support and the development of better and more appropriate coping skills for that given situation. In these situations, yoga, meditation, and exercise may be extremely efficient in addressing stressful situations whereas psychotherapy can be effective in developing better coping skills. In many instances, it is not necessarily the fact that a person’s anti-depressant or anti-anxiety medication is not working, the fact of the matter is that the person’s life is still a mess and they need to begin to put it in order. Unless the person is able to address these matters, the likelihood of a person responding effectively to a pharmacological intervention is going to be minimal.It is safe to say that one’s mental health and sense of well-being is not a given in anyone’s life. Just because a person has a positive outlook on life, doesn’t mean that their genetic make-up couldn’t play a factor in that person’s level of functioning. Or, the person who has savvy coping skills in dealing with incredible amounts of stress, doesn’t mean that the accumulative effects of those stressors will not take a physiological toll on that person via heart disease or cancer.
Maintaining mental health and well-being needs to be worked at on an on-going basis, not too different than an athlete needs to train to maintain peak performance. In the arena of mental health and well-being, a person needs to monitor and train how they are performing in the areas of neurobiology, stress reduction, and the development of more effective and positive coping skills. The ability of a person to attend to these areas through the use of yoga, nutrition, exercise, diet, meditation, stress reduction techniques, psychotherapy, hypnosis, just to name a few approaches, the greater likelihood the person will maintain that sense of well-being. A question that a person needs to ask themselves is what is it they are doing to ensure the balance of these three key areas of their life.
For over 25 year, Thomas G. Beley, PhD, LCSW has worked in the field of addictions and mental health. Over these two-and-a-half decades of helping people who struggle with mental health and substance use disorders, he has proven to be an expert clinician and innovative and compassionate leader. Palm Healthcare Company is proud to have an executive team with experience and incredible commitment to helping others. If you or someone you love is struggling, please call toll-free now. We want to help.
CALL NOW 1-888-922-5398
by Justin Mckibben | Jan 25, 2018 | Acupuncture, Addiction Medicine, Addiction Treatment, Anxiety Disorder, Holistic Treatment
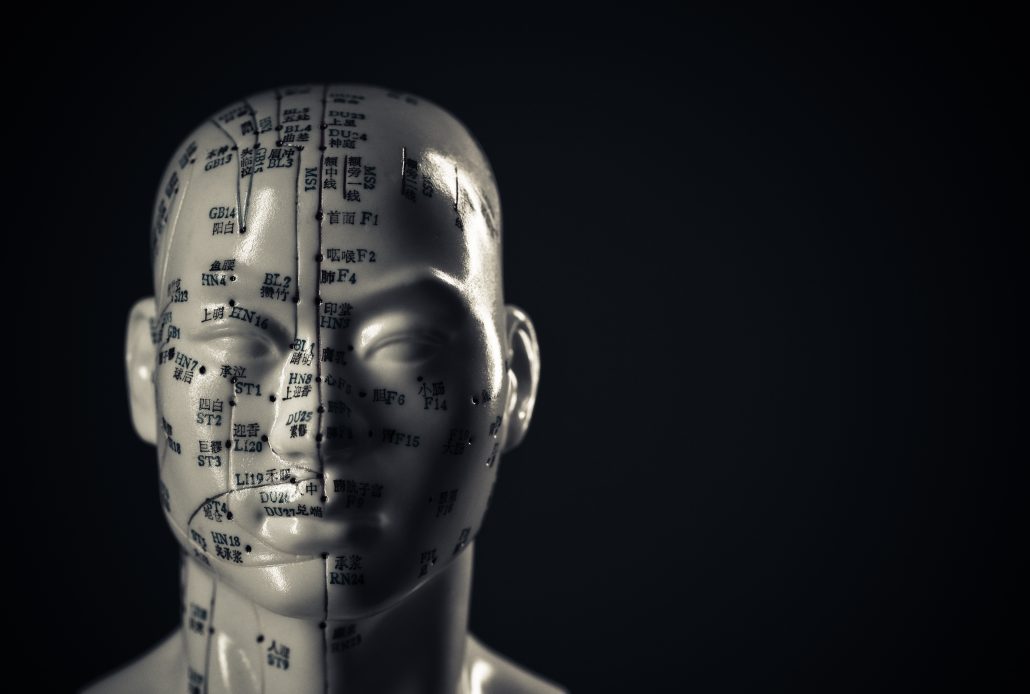
To put it simply, acupuncture is a form of alternative medicine in which thin needles are inserted into the body. This practice is a key component of traditional Chinese medicine, and the most widespread method of acupuncture in the United States derives from traditional Chinese medicine. Acupuncture therapy has been used to help heal and promote wellness for over 2,000 years.
Modern medicine explains the benefits of acupuncture using neuroscience. Traditional Chinese medicine focuses on the balance and flow of energy. Western practitioners tend to identify acupuncture points as places where stimulation to nerves, muscles, and connective tissue increases blood flow and activates the body’s natural endorphins. There are critics who say many studies on acupuncture are hard to prove because of the nature of the treatment versus control groups. Some would say any improvements may merely by placebo effects. However, many have experienced benefits from trying this method of treatment as part of personalized addiction recovery programs.
It is typical to use acupuncture for pain relief, although it can help with a wide range of other conditions as well. Generally, acupuncture is used in combination with other forms of treatment and has been known to be an effective addition to holistic addiction treatment. In 1997, the U.S. National Institute of Health (NIH) publicized acupuncture’s safety and efficacy for helping treat various conditions.
Relapse and Craving Prevention
One acupuncture technique applies small needles called “seeds” to the ear. A large study examining three auricular acupuncture protocols such as this looked at relapse prevention in drug users. This study concluded that all three protocols were associated with reductions in drug use over time.
In another study examining acupunctures impact on relapse prevention, an 8-week randomized study of 32 subjects compared two groups:
- One group was given acupuncture treatment with two prescription medications used for craving reduction
- The other received a placebo for cocaine addicts on methadone maintenance therapy
Half of the subjects in the test dropped out, so the results were not so concrete. However, almost 90% of those who completed the treatment achieved abstinence by the end of the study. The patients who completed the trial and achieved abstinence reported:
- Diminished craving
- Significantly improved mood
Over the years there have been hundreds of clinical studies on the benefits of acupuncture. According to the UC San Diego Center for Integrative Medicine, some studies claim that it can successfully help treat:
Although again, these treatments can often include medications and other forms of therapy.
Opiate Addiction and Acupuncture
The mesolimbic dopamine system originates in the ventral tegmental area (VTA) and projects to regions that include:
- Nucleus accumbens
- Prefrontal cortex
Expert believe these areas play a pivotal role in the development of opiate addiction.
Opioid abuse causes changes in the levels of dopamine in the brain. These reactions are typically associated with feelings of pleasure and well-being. This positive association helps drive the development of opiate abuse. So when someone discontinued opioid use, it reduces dopamine outflow in the nucleus accumbens. This is what creates opioid withdrawal.
Many studies in animals and humans have demonstrated that acupuncture causes multiple biological responses. The best-known mechanism is via endogenous opiates and their receptors.
In 1993, Han and Zhang reported the effectiveness of EA on morphine abstinence syndrome in a rat experimental model. The authors found that acupuncture point 100 Hz EA produced a statistically significant suppression of symptoms such as:
- Wet shakes
- Teeth chattering
- Escape attempts
- Weight loss
They also discovered acupuncture point 2 Hz EA produced a mild but significant suppression in:
- Escape attempts
- Wet shakes
These results suggest that 100 Hz EA was far more effective than 2 Hz EA in suppressing drug withdrawal syndrome. Further studies suggested that EA suppresses opiate withdrawal syndrome by activating κ opioid receptors and dynorphin release.
In short, there are researchers who believe that acupuncture is an effective method of therapy for helping treat those recovering from opioid addiction. Again, it may not be a good enough treatment on its own, but it can have an impact on cravings and other stressors in the body that help prevent relapse. So whether you believe in balancing the flow of energy in the body, or just pinpointing the nerves, acupuncture might be one way to enhance your recovery program.
Palm Healthcare Company offers acupuncture therapy as one of the many holistic treatment options to help each individual customize their own recovery plan. Acupuncture provides another opportunity to cultivate a state of physical and mental wellness in addiction recovery. Everyone struggling deserves a chance to be as healthy and happy as possible while overcoming drugs or alcohol. If you or someone you love is struggling, please call toll-free now.
CALL NOW 1-888-922-5398
by Justin Mckibben | Jan 22, 2018 | Donald Trump, Drug Abuse, Drug Policy, Law Enforcement, News, War on Drugs

For the last few years federal politicians, local officials, and addiction advocates have spoken a great deal about the critical condition of the opioid crisis in America. Just a few months ago President Trump declared the opioid epidemic a public health emergency, and his administration had created a special White House Opioid Commission to do extensive research and community outreach to try and better understand the problem and offer possible solutions.
Now recent reports state that President Donald Trump is actually planning to cut the budget of the Office of National Drug Control Policy.
The Office of National Drug Control Policy (ONDCP) just happens to be the top office responsible for coordinating the federal response to the opioid crisis. This plan is being noted as his administration’s second attempt to gut the ONDCP, so how would this change the current system?
What is the Plan?
So what does this mean? If President Trump were to go forward with this proposal, it would shift the office’s two main grant programs. These are:
- The High Intensity Drug Trafficking Areas grant
- The Drug Free Communities Act
According to POLITICO, multiple sources in the administration and others working with the government on the opioid crisis said those resources would then be given respectively to:
- The Justice Department
- Health and Human Services Department
According to a document from the Office of Management and Budget, this proposal would cut 95% of the ONDCP’s budget. Officials in President Trumps administration say that the approximately $340 million in grants will be administered by larger agencies. But the ONDCP will still serve as the White House’s drug policy shop. But the ONDCP will still be the main resource for President Trump for drug policy.
According to the proposal, President Trump and his administration believe these programs are just duplicates of other initiatives. This cut would also result in the ONDCP losing up to 33 employees. Skeptics say taking these resources leaves the policy office with little power or purpose.
Some Support President Trump Plan
Not everyone believes this is a bad idea. Some advocacy organizations are cautiously optimistic that changes to the ONDCP could actually end up being a good thing. One of them is the Drug Policy Alliance. They believe the opioid epidemic has continued to get worse under the ONDCP, and that maybe a shift in perspective is necessary to make a difference.
Grant Smith, deputy director of national affairs for the Drug Policy Alliance states,
“The reality is that ONDCP is an agency in dire need of reform,”
Smith believes that the particular grant programs mentioned previously “are a phenomenal waste of money that contribute to the incarceration and stigmatization of drug users.”
They are also afraid President Trump would use a more powerful Drug Czar to aggressively treat drug abuse as a criminal justice issue rather than as a public health problem. If so, it might be a good idea to take the power of these grants out of the executive branch’s control.
Some believe the ONDCP won’t be particularly helpful for the future of drug policy due to some of the organizations part positions, such as denying medical use of marijuana or encouraging the expansion of workplace drug testing. There have been stories questioning the 24-year-old deputy chief of staff President Trump appointed to head the ONDCP. Some see having an individual with no drug policy experience running this important agency as an indication of inconsistnecy.
Supporters of moving the grants and cutting the ONDCP say it would decrease overlap since the DOJ already works on drug trafficking and HHS also has substance use prevention. This may not be the worst assumption either, considering that President Trump and his administration have touted a law-and-order approach that has many concerned about further stigmatizing and punishing those in need of help.
An OMB spokesperson stated,
“DOJ and HHS are both major grant management organizations that can look holistically at allocations across law enforcement and drug prevention and treatment resources.”
So some are hopeful it could just put the grants under a different roof. But critics say these programs are working, and it is hazardous to try and dramatically restructure them at such a desperate time.
Other Republicans Rebuke the Plan
Health policy experts, lawmakers, and even fellow Republicans are unhappy with this latest proposal. Some even say this is just one example of a series of actions showing that President Trump’s administration isn’t serious about addressing the opioid epidemic.
Last year the White House Office of Management and Budget proposed completely cutting these grants. However, that proposal was met with intense resistance from both Republican and Democratic lawmakers. Now, health experts and officials from both sides are speaking out against this plan. Regina LaBelle, who served as ONDCP Chief of Staff during the Obama administration, states:
“I’m baffled at the idea of cutting the office or reducing it significantly and taking away its programs in the middle of an epidemic,”
Many are already expecting lawmakers to push back again against this plan from President Trump.
Republican Senator Shelley Moore Capito from West Virginia, a state ravaged by opioids, told POLITICO she will “resist that move”. Capito also says she believes the grants should be kept at ONDCP. This would keep them within the executive branch and under the president’s purview.
Republican Senator Rob Portman from Ohio, another state that has been hit hard by the opioid epidemic, said he also plans to fight back against the proposed cuts. Portman says the anti-drug programs the administration wants to cut have done an immense amount of good in Ohio.
Going Against Opioid Commission
President Trump established the White House Opioid Commission to make recommendations on addressing the opioid crisis. Now even advisors on this panel are saying this new move goes against the opioid commission’s recommendations.
Former Representative Patrick Kennedy, a member of the opioid advisory commission, said the panel advised President Trump to fortify the ONDCP, not defund it. The opioid commission had also endorsed both of these grants as crucial to overall response efforts. Kennedy went on to say,
“It guts the two main purposes of ONDCP… It really undermines the mission.”
So there are those that think changing the ONDCP could be a necessary sacrifice to make progress. However, others are concerned that it is not the right move, and definitely not the right time.
We should note that the proposal from President Trump is subject to change. There is still more time to learn about how moving money from the Office of National Drug Control Policy could impact the governments work against the opioid crisis. Could this change refine the process of accessing these grants? Or could it cripple an important agency for fighting addiction during of one of the country’s worst drug outbreaks? Hopefully, these changes can be managed in a way that creates new opportunities instead of removing them.
Providing support and life-saving resources is vital to overcoming addiction. Every day people are struggling with drug or alcohol use disorders, and some of them never find the help they need. Safe and effective addiction treatment is one of the best tools we have. If you or someone you love is struggling, please call toll-free now. We want to help.
CALL NOW 1-888-922-5398
by Justin Mckibben | Jan 19, 2018 | Anxiety Disorder, Coping Skills, Dual Diagnosis, Mental Health, News, Opioids, Prescription Drugs, Suicide

Over the last 15 years, the suicide rate has climbed by an estimated 32%. While the overdose deaths in relation to the opioid crisis have become a constant issue around the country, some researchers suggest that the real suicide rates are even higher, but some of them are being misclassified as overdoses.
So, are more people dying due to drug abuse, or are more people taking their own lives using powerful street drugs and prescription narcotics?
Studying Suicide and Drugs
The idea that many of the deaths recorded as opioid overdoses may have been suicides, according to the researchers, is due to a significant gap between suicide rates and intoxication mortality rates.
A study from the Luskin School of Public Affairs at the University of California, Los Angeles, was published in the journal PLOS One. This study states that both suicide and drug intoxication death rates in the United States have risen over a period of 15 years. Researchers compiled data from the Center for Disease Control and Prevention (CDC) to show:
- 2000- The suicide rate was 10.40 per 100,000 people
- 2015- Suicide rate rose to 13.75 deaths per 100,000 people
- 2000- Drug intoxication mortality rate for those over the age of 15 was 7.81 deaths per 100,000
- 2015- Drug intoxication death rate for those over the age of 15 rose to 20.07 per 100,000 in 2015
This means that the drug intoxication death rate rose by 257% in those 15 years, while suicide rates only rose by 32%. While 32% is still a devastating number when it comes to such a tragic circumstance, there is still a huge difference between 32% and 257%. These researchers believe this major difference in the reports of mortality rates suggests a lack of suicide reporting.
Difficulties in Death Investigation
One of the big problems, according to the study’s author Mark Kaplan, is resources. Kaplan is a professor of social welfare at UCLA, and he stated to local news sources,
“Unfortunately, part of the problem is due to serious under-resourcing of state and local death investigation systems throughout most of the U.S.
“Many of these deaths were probably suicides, yet reported as accidental self-poisoning rather than intentional self-harm, particularly among the middle-aged.”
The study by Kaplan and his colleagues further explains that when it comes to suicide by overdose, things like an individual’s psychiatric history or the presence of a suicide note are crucial to helping professionals identify a death as a suicide.
“A suicide note, prior suicide attempt or affective disorder was documented in less than one-third of suicides and one-quarter of undetermined deaths,”
“Our incorporation of undetermined deaths, as well as registered suicides, not only provided a window on the nature of suicide misclassification within the undetermined death category but within the accident category—as a much larger reservoir for obscuring drug intoxication suicides.”
So by acknowledging that there is not always an obvious indication that a death is a suicide, even in cases that are classified in suicide, the researchers believe that many deaths that involved drugs have most likely been categorized as overdoses instead of making a deeper inquiry into the circumstances surrounding an individual’s death.
Opioids Causing Ambiguity
With the opioid crisis in America, it has become even more difficult to measure the suicide rates. And that isn’t just this research teams opinion either.
In 2015, the CDC hosted a meeting to address the challenges presented for medical examiners and coroners across the country. The primary focus was concerning cases of fatal intoxication due to opioids and other drugs. The summary of this meeting concluded that drug intoxication deaths may be among the most difficult to determine regarding the manner of death. The summary notes that reasons for such difficulty in having a more accurate manner of death include:
- Potentially equivocal evidence
- Intent to die
- Overlapping demographic groups affected
- Overlapping premorbid risk factors (e.g., substance abuse, mental health problems).
Opioid addiction, much like any other form of substance use disorder, is often closely connected to other issues, including anxiety, trauma and mental health disorders. Some individuals living with mental health conditions who abuse opioids may be self-medicating and accidentally overdose. But others may be suffering so severely, with conditions like depressive disorders or bipolar disorder, that they ultimately take their own lives intentionally with the powerful drugs. With opioid abuse being so widespread and devastating, the line between the two has begun to blur.
Both studies mentioned clearly indicate in order to truly comprehend an accurate number of suicides by overdose, more research is needed. Both also admit that the number may never be exact.
Even though we will probably never have a definitive answer, the question is still important to ask. By knowing whether opioid deaths are caused by accidents or intentional we can develop better strategies to provide education and prevention.
This is also why mental health should always be a priority when it comes to addiction treatment.
Substance use disorder and suicide are both connected to mental health and personal wellness. Too often they both lead to avoidable tragedies. Therefore, mental health and wellness should be a priority for addiction treatment. If you or someone you love is struggling with substance abuse or addiction, please call toll-free now.
CALL NOW 1-888-922-5398
by Justin Mckibben | Jan 9, 2018 | Addiction Stigma, Drug Abuse, Opioids, Prescription Drugs, Professionals, Stigma
(This content is being used for illustrative purposes only; any person depicted in the content is a model)
The opioid crisis has affected every community in America. Opioids affect rural working class people, those in the inner city and suburbs, or even the wealthy and well-to-do professionals. While drug abuse in business has been highlighted in blockbuster films like the Wolf of Wall Street, the current reality is not far from it. According to addiction experts, substance use disorder is making a sobering impact on the financial industry.
This comes from not just an upscale partying lifestyle, but also from drugs used to manage performance and stress, along with physical pain. According to addiction experts, the financial industry itself is actively turning a blind eye to the issues concerning opioid abuse on Wall Street because money is still the priority, and stigma still gets in the way.
Opioids on Wall Street: White-Collar Confessions
As it stands there is no comprehensive research that takes a detailed look at opioid abuse in Wall Street among finance professionals. So we can’t exactly show the numbers to prove it’s prevalence. However, what we see consistently is a dramatic increase in addiction and overdose rates all over the nation in recent years.
Luckily, professionals from this demographic are beginning to speak out in hopes of progressive change.
One such individual is Trey Laird, a former Wall Street trader, who recently spoke to CNBC about his six-year opioid addiction. During the conversation Laird reiterates the critical understanding that substance use disorder can reach anyone, saying:
“Addiction pervades every single socioeconomic demographic that there is. Every industry, every race, men, women. It doesn’t care who you are,”
After getting clean himself, Laird went on to open a sober living community and says he hopes to specifically serve the Wall Street and white collar demographic.
According to Laird, there has been more talk about opioid addiction among people in higher socioeconomic brackets, but there is still much work that needs to be done. He acknowledges that increasing awareness is doing a great deal, but that the problem is also at an increase. Wall Street may finally be talking about it, but how many professionals will get the help they truly need?
Opioids on Wall Street: Stocks and Stigma
One of the biggest obstacles facing white-collar workers like those in Wall Street is the engrained stigma still attached to addiction. Even with all the shifts in our culture toward a better understanding of substance use and the compassion for those struggling, professionals still have this seemingly unbearable hurdle in front of them.
Truthfully, stigma is something that prevents most people from getting help. Professionals will often be too afraid of losing their jobs to admit they need help. Many in the world of Wall Street and finance may have no information on how to seek out treatment while adhering to their professional boards’ guidelines and business practices.
With white-collar workers, this may be an especially difficult thing because the idea of addiction is so often attached to stereotypes of the unemployable, the homeless, the unreliable and unstable that their high-earning careers might minimize the impact drugs have on their lives. Wall Street stockbrokers and traders might not see themselves as having a problem as long as they can function, which brings in the idea of the “functioning addict.”
Opioids on Wall Street: Function Addiction is Still Addiction
Many white-collar workers who struggle with drugs or alcohol may consider themselves a “functioning addict”, meaning they are less likely see their actions as a problem because they are able to maintain their professional or even personal lives. To make matters worse, frequently the people around someone who is professionally successful will not believe the addiction is real. They may admit that you’ve been careless or destructive in some respects, but will ultimately minimize it due to your financial stability.
As long as you’re making money and paying the bills how could you possibly be “that bad?”
Well, because “functioning addiction” is still an addiction.
Addiction isn’t about whether or not you are able to hold down a steady income. It does not depend on whether or not other people recognize that you have a problem or your competence with your profession. While addiction can and will have an impact on these things, it isn’t always as black and white as most people like to pretend.
Notice how earlier we said you may “maintain” other areas of your life? Well, we mean to say that you can get by for a while, but eventually, the effects of addiction will catch up with you. It could be in the form of serious health consequences or other devastating circumstances. It could take days, months or even years, but it will leave a mark.
Sadly, “functioning addicts” are also far less likely to get the help they desperately need.
Opioids on Wall Street: It Could Be You
While you might be able to keep your addiction secret, in the beginning, things will eventually get worse. Eventually, your addiction will become unmanageable.
If you think you might fit the “functioning addiction” criteria, look at the following questions and answer them honestly.
- Do you often think about using drugs or drinking?
- Do you find it hard to stop after you start drinking or using?
- Are you scheduling your time around drinking or using drugs?
- Have you tried to stop before, but found that you were unable to?
- Do you drink or use drugs first thing in the morning?
- Are you drinking or using drugs at work?
- Do you hide your drug use or drinking?
- Have you done something risky, like driven drunk?
- Do you worry about your drug use or drinking?
If you find you are answering “yes” more than “no” then you should seriously consider speaking with a medical or addiction professional about your drug use or drinking.
The opioid crisis is nothing to be ignored. Despite all that we think we have learned about addiction too many professionals don’t get the help they need. No one is exempt from the destruction of addiction. Opioids don’t care what street you work on, Wall Street or not, they can ruin your life all the same. If you or someone you love is struggling, please call toll-free now. We want to help.
CALL NOW 1-888-922-5398