Palm Healthcare Company Presents The Pain Recovery Program

(This content is being used for illustrative purposes only; any person depicted in the content is a model)
Palm Healthcare knows the importance of addressing the multi-faceted needs of the individual who suffers from chronic pain. This is why we created the Pain Recovery Program. A person in pain is not only concerned about reclaiming their own sense of well-being and functioning. They are also concerned about reclaiming their sense of purpose, independence, and direction to life.
Palm Healthcare Pain Recovery Program
The focus of the Pain Recovery Program is assisting that person in pain in reclaiming all aspects of their life. Palm Healthcare utilizes a comprehensive bio-psychosocial perspective while incorporating the latest holistic, traditional, and state of the art, non-invasive technology and interventions.
Individuals participating in The Pain Recovery Program are provided a variety of treatment options that include:
- Medication management
- Nutraceutical (vitamin) therapy
- Physical therapy
- Strength and conditioning
- Massage
- Muscle manipulation therapy
- Chiropractic care
- Aquatic therapy
- Hypnotherapy
- Biofeedback
Each person in The Pain Recovery Program will receive a personalized treatment plan based on comprehensive evaluations and the specific needs of the individual and their specific needs.
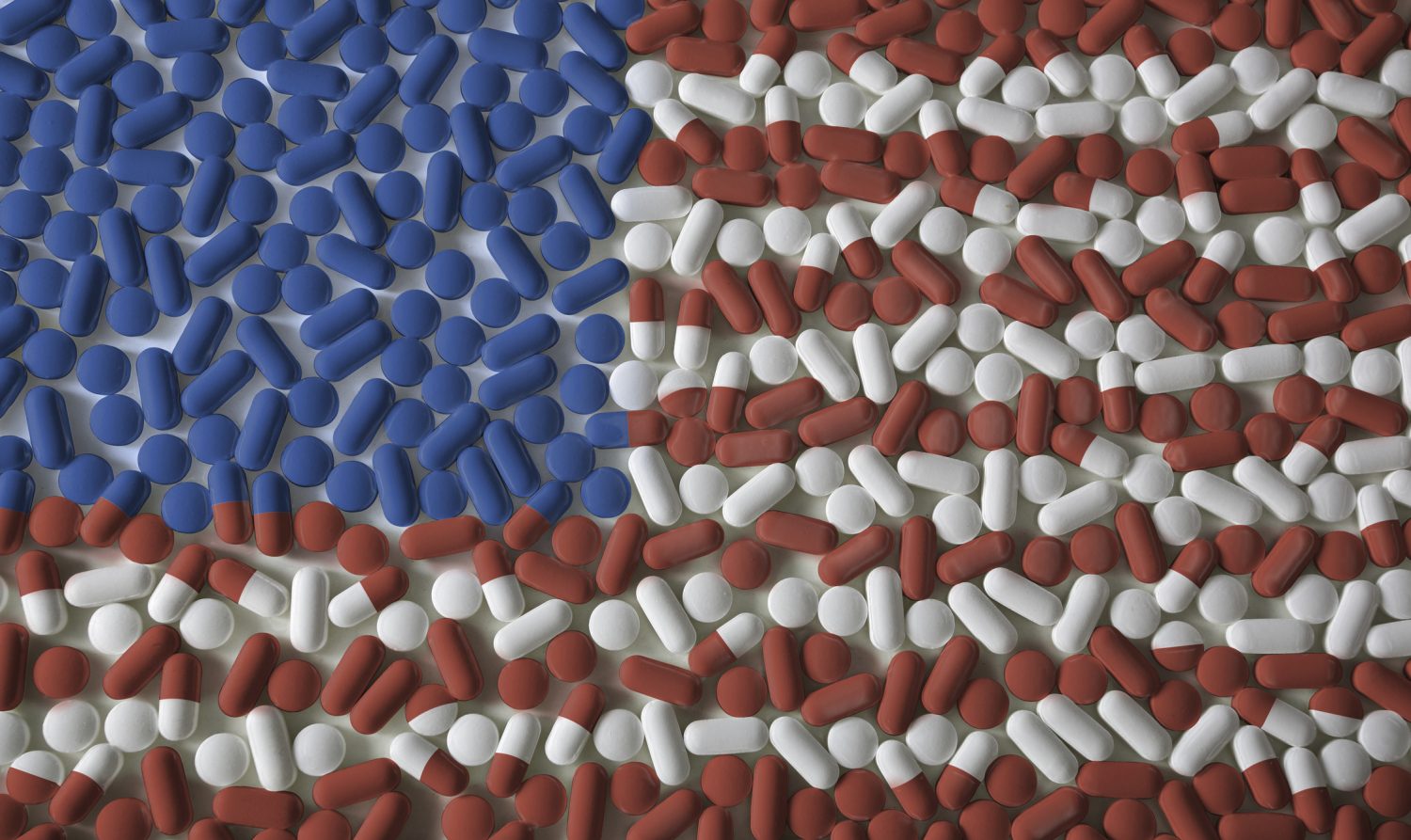
Connecting Pain and Addiction
Part of overcoming pain while overcoming addiction is understanding how the two are so closely related. Patients who are struggling with one or both of these conditions often report adverse symptoms such as:
- Insomnia
- Depression
- Impaired functioning
- Anxiety
Chronic pain and substance use disorder (SUD) have similar physical, social, emotional, and economic effects on health and well-being; one can easily be confused for the other, while both can exacerbate each other.
Pain in the Brain
Chronic pain and addiction actually have many of the same exact neurophysiological patterns.
For instance: Chronis pain involves abnormal neural processing. Coincidentally, addiction results when normal neural processes are altered into dysfunctional patterns, including disruptions in:
- Memory
- Reward systems
- Stress responses
The truth is, there is still a lot to learn about both of these conditions, including patterns of severity, the course of development and responses to treatment.
Emotional Responses
Gauging and effectively addressing emotional responses is also crucial to effective and lasting pain treatment.
Pain and Emotions
Continued pain can also cause emotional responses, such as:
- Sleeplessness
- Anxiety
- Depressive symptoms
Each of these experiences can even turn into more pain. Even after these psychological causes have been addressed the feedback effect can still cause pain in the body.
In fact, there are many studies that indicate pain treatment has worse outcomes when depression is a factor. Some experts say you can even predict how a pain syndrome will evolve based on the emotional status of the patient.
Emotions and SUD
With substance use disorder, the individual’s emotional state is a core cause of continuous drug use. People who use drugs often experience these same emotional responses like anxiety and depression as a result of isolation, social and professional hardships and other side-effects of their drug use. Not to mention the way certain drugs impact the brain. Emotional and psychological trauma can be just as severe for these individuals as physical trauma.
On the other hand, some people may already have a history of experiencing these emotional difficulties and actually be trying to treat themselves by abusing drugs. This feeds into the cycle of emotional distress and substance use.
Complicated Relationship
Both addiction and chronic pain fluctuate in intensity with time under different circumstances. Depending on what is going on in someone’s life, their pain may get worse or seem to disappear, just like an addiction may seem controllable for a time before hitting another harsh bottom.
Both often require ongoing management. But the difficulty can also be that these two conditions feed into each other in a very complicated, and at times toxic, relationship.
Treatment for one can either support or conflict with the other.
The Painful Cycle of Addiction
One of the many difficulties many people experience when trying to overcome addiction while struggling with chronic pain syndrome is that there is a cycle of pain- drugs- more pain- more drugs that seems inescapable.
For example- Narcotic medication typically prescribed for chronic pain may be an issue for someone with a history of substance use disorder.
But then if someone uses a narcotic prescription pain medication, such as opioid analgesics, it can create a physical dependence. Then when the substance is absent from the body the withdrawal symptoms set in.
Withdrawal and Pain
Withdrawal symptoms frequently lead to an increase in symptoms of anxiety and depression, while creating even more physical pain. In turn, the anxiety and depression from withdrawal can contribute to that pain even further.
This pain and distress can provoke a severe obsession with whatever substance the individual was relying on to provide relief. In other words, the individual will crave the drug even more because they are not only experiencing the psychological distress from their brain lacking the drug, they are also experiencing a magnified sense of pain from the experience as well.
Again, the cycle of pain- seeking relief from the pain through substances- recurring pain- continued substance use making the problem worse. The Pain Recovery Program is about interupting this self-destructive cycle with new, sustainable methods of pain management.
The Importance of Treating Pain and Addiction
Substance use disorder in relation to prescription pain medication is widely misunderstood, and while some programs focus on treating the addiction, if there is no way of addressing the chronic pain it does not help the chances of successful recovery. Part of working with chronic pain patients struggling with addiction is education on both conditions while providing effective treatment opportunities simultaneously.
Providing pain management opportunities for the U.S. population struggling with substance use disorder is a unique challenge for many primary care physicians. That is why experienced professionals in the field of drug and alcohol addiction treatment are in a unique position to help.
First, we need to acknowledge a few issues, including:
- People recovering from addiction experiencing pain are less likely to receive adequate pain management than anyone else.
- Insufficient pain relief is a substantial risk factor for possible relapse into substance use.
- It is crucial to distinguishing between patients who are seeking relief for legitimate pain and those who are seeking pain medication for recreational abuse
- Psychiatric and medical illnesses can complicate effective pain management
Experts believe that addiction specialists, in particular, can make significant contributions to the management of chronic pain in patients who suffer from substance use disorder. Addiction specialists can:
- Help create safeguards to assure any pain medication is taken appropriately
- Reinforce behavioral and self-care components of pain management
- Help individuals with strategies to reduce stress
- Assess patients’ recovery support systems
- Help to understand and identify relapse risks
Chronic pain management can be a complex process. Experts say that the efficiency of treatment is amplified when all medical and behavioral healthcare professionals involved collaborate as a team. Palm Healthcare Company’s Pain Recovery Program is all about a united effort toward treating both conditions with a variety of experienced professionals and trainers.